Antibiotics in Children: When They're Needed, Side Effects, and Allergy Risks
Every parent has been there: your child has a fever, a runny nose, and won’t eat. You know they’re sick, but you’re not sure if it’s a virus or something bacterial. And then the question comes up - antibiotics or not?
The truth is, most childhood illnesses don’t need antibiotics at all. Yet, too many kids still get them - and that’s putting their health at risk in ways most parents don’t realize.
Antibiotics Only Work on Bacteria - Not Viruses
Antibiotics are powerful drugs, but they’re not magic pills. They only kill bacteria. That means they do nothing for the common cold, flu, most sore throats, or stomach bugs. Those are caused by viruses. And giving antibiotics for viruses doesn’t help your child get better faster. It just adds risk.
Here’s what actually needs antibiotics in kids:
- Strep throat (confirmed by a rapid test or culture)
- Ear infections with moderate to severe pain or fluid draining from the ear
- Bacterial sinus infections lasting more than 10 days with worsening symptoms
- Pneumonia when a doctor suspects bacteria (not all cases)
- Whooping cough (pertussis)
That’s it. About 20% of sore throats, 10% of pneumonia cases, and a small fraction of ear infections are bacterial. The rest? Viral. And for those, antibiotics are not just useless - they’re harmful.
Common Side Effects: It’s More Than Just Upset Stomach
Side effects from antibiotics are common. In fact, about 1 in 10 children experience them. Most are mild, but they’re annoying - and they can be misleading.
Diarrhea is the #1 side effect. It happens in 5% to 25% of kids, depending on the antibiotic. Amoxicillin, the most common one, causes it often. Nausea, vomiting, and loss of appetite are also frequent. These aren’t signs the medicine isn’t working - they’re just how the body reacts to the drug.
Then there’s the yeast infection. Yes, even in kids. Antibiotics kill good bacteria in the gut - and that lets yeast grow unchecked. That means diaper rash that won’t go away, or in older kids, a sore, itchy mouth (thrush). It’s not rare. About 1 in 20 kids on antibiotics get it.
And here’s what most parents don’t know: a rash isn’t always an allergy. About 80% of rashes that show up during antibiotic treatment are just side effects - not true allergies. They’re flat, pink spots, not raised or itchy. They usually go away on their own. But if your child gets hives, swelling of the lips or face, trouble breathing, or wheezing - that’s a real allergic reaction. And it needs immediate medical attention.
True Allergies Are Rare - But Often Mistaken
Many parents say, “My child is allergic to penicillin,” based on a rash they got years ago. Or maybe a sibling had a reaction. But here’s the shocking truth: 95% of kids labeled “allergic to penicillin” can actually take it safely.
True penicillin allergy - the kind that causes anaphylaxis - is extremely rare in children. Less than 1 in 2,000 courses of amoxicillin leads to a life-threatening reaction. But because of mislabeling, kids are often given stronger, more expensive antibiotics that cause more side effects and fuel resistance.
Don’t assume. If your child was told they’re allergic, ask your doctor about allergy testing. It’s simple, safe, and can change how they’re treated for the rest of their life.

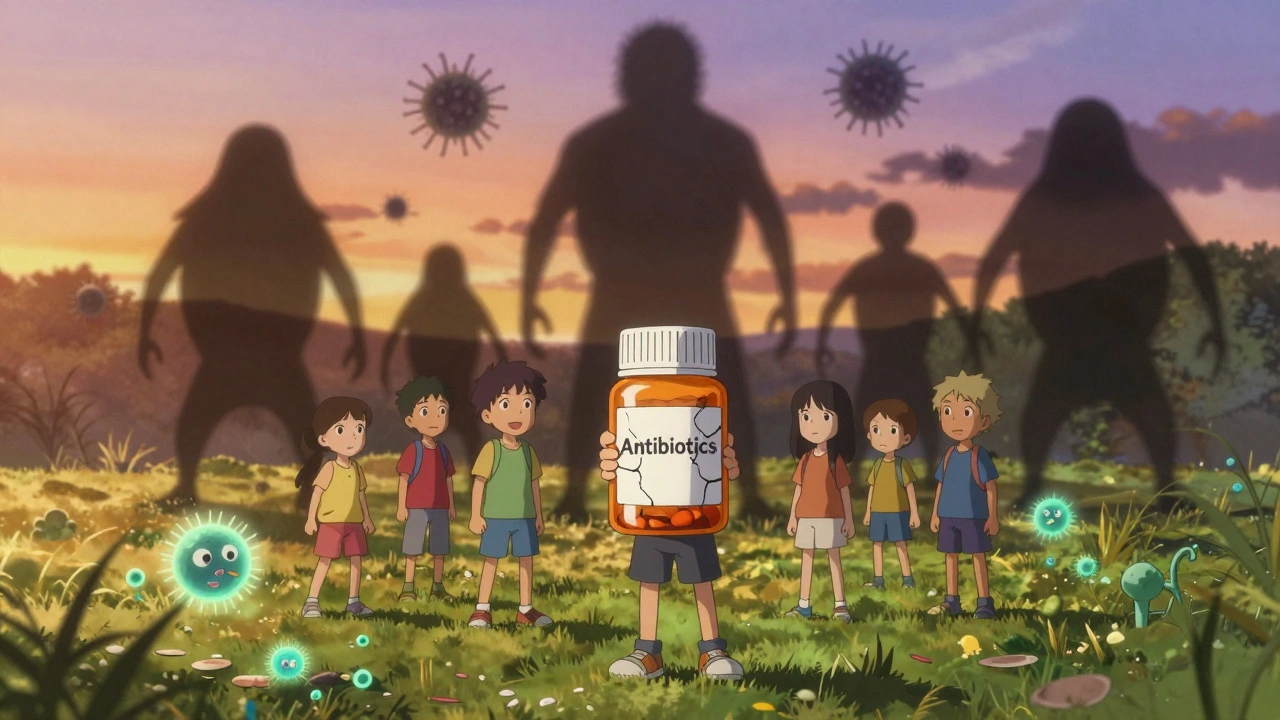
Why Overuse Is Dangerous - And Getting Worse
Every time you give an antibiotic when it’s not needed, you’re helping bacteria become stronger. That’s antibiotic resistance. And it’s not a future problem - it’s happening now.
Here’s what’s changed in the last decade:
- 47% of the bacteria that cause ear infections and pneumonia are now resistant to penicillin - up from 35% in 2013.
- MRSA infections in kids have jumped 150% since 2010. Many are caught in the community, not hospitals.
- 30% of antibiotic prescriptions for kids are unnecessary, according to the CDC.
This isn’t just about your child. It’s about all of us. When bacteria become resistant, the drugs stop working. That means simple infections could become deadly again. Right now, antibiotic-resistant infections cause over 35,000 deaths a year in the U.S. alone. And kids are part of that.
When to Wait - And When to Act
Not every fever or cough needs antibiotics. Doctors now use “watchful waiting” for many cases.
For ear infections in kids 6 to 23 months with mild symptoms on one side? Wait 48 to 72 hours. If the pain doesn’t get worse, and the fever drops, antibiotics often aren’t needed. Many ear infections clear up on their own.
For sinus infections? If it’s been less than 10 days, it’s probably viral. If symptoms get worse after 5 days, or last longer than 10 days with thick yellow or green mucus, then it might be bacterial.
And for sore throats? Never guess. A rapid strep test is required. Clinical symptoms alone are wrong more than half the time. Don’t let your child be treated based on a guess.
There’s new tech helping doctors make better calls. A simple blood test called CRP can tell if an infection is likely bacterial or viral - and clinics using it have cut unnecessary antibiotics by 85%.
How to Give Antibiotics Right - And What to Avoid
If your child is prescribed antibiotics, here’s how to get it right:
- Give the full course - even if they feel better in 2 days. Stopping early lets the toughest bacteria survive and multiply.
- Follow the schedule. Amoxicillin is usually twice a day, 12 hours apart. Don’t skip doses.
- If your child vomits within 30 minutes of taking it, give the full dose again. If it’s 30 to 60 minutes after, give half.
- Don’t mix antibiotics with large meals. It can interfere with absorption. A small spoonful of applesauce or chocolate syrup can help hide the taste - but avoid dairy with some antibiotics like tetracyclines (rarely used in young kids).
- Watch for improvement. If there’s no change after 48 to 72 hours, call the doctor. The antibiotic might not be right.
And please - don’t save leftover antibiotics for next time. They expire. They might not be the right drug. And using them without a diagnosis can make things worse.
What Parents Should Know - But Often Don’t
Green or yellow snot? Normal in a cold. It doesn’t mean antibiotics are needed.
A fever that lasts 3 days? Doesn’t mean bacterial. Most viruses run for 7 to 10 days.
Pressure from other parents? You’re not alone. Many feel forced to ask for antibiotics. But the best thing you can do is ask: “Is this definitely bacterial? Do we need an antibiotic?”
And remember: time and comfort care are powerful. Rest, fluids, fever reducers like acetaminophen or ibuprofen, saline drops for noses - these help more than antibiotics for viral illnesses.
What’s Changing - And What’s Next
Doctors are getting smarter. New tests can now tell in 6 hours whether bacteria are resistant to certain drugs - instead of waiting 2 to 3 days. That means kids get the right antibiotic faster, and avoid broad-spectrum ones that cause more side effects.
Studies show that using a blood marker called procalcitonin cuts unnecessary antibiotic use by 62% without increasing complications. That’s huge.
By 2025, the CDC aims to cut inappropriate antibiotic prescriptions in kids by 50%. That’s possible - but only if parents and doctors work together.
The most powerful tool we have for most childhood illnesses isn’t a drug. It’s patience. It’s rest. It’s knowing when to wait.
Antibiotics save lives. But only when they’re used right. Protect them. Protect your child. And protect the next generation from a world where common infections can’t be treated.
Can antibiotics make my child’s diarrhea worse?
Yes. Antibiotics kill both harmful and helpful bacteria in the gut, which can lead to diarrhea. In some cases, this can trigger a more serious infection called Clostridium difficile (C. diff), especially after long or repeated antibiotic use. If your child has severe, watery diarrhea, fever, or stomach cramps during or after antibiotics, contact your doctor immediately.
Is it safe to give my child antibiotics with food?
It depends on the antibiotic. Amoxicillin and cephalosporins can be given with food to reduce stomach upset. But some, like tetracyclines, must be taken on an empty stomach - though these are rarely used in young children. Always check the label or ask your pharmacist. A small snack is fine for most pediatric antibiotics - just avoid large meals that might delay absorption.
My child had a rash after amoxicillin. Does that mean they’re allergic?
Not necessarily. About 80% to 90% of rashes from amoxicillin are non-allergic side effects - especially if they’re flat, pink, and not itchy. True allergic reactions include hives, swelling of the face or lips, wheezing, or trouble breathing. If your child had a mild rash with no other symptoms, talk to your doctor about allergy testing before assuming they’re allergic for life.
Can I use leftover antibiotics from a previous illness?
No. Antibiotics are prescribed for a specific infection, dose, and duration. Using old medicine could be the wrong drug, wrong dose, or expired. It might not work - or worse, it could make the infection worse or cause side effects. Always get a new prescription if your child is sick again.
How long should I wait before calling the doctor if antibiotics aren’t working?
If your child shows no improvement after 48 to 72 hours - or if symptoms get worse - contact your doctor. Fever that returns, increased pain, trouble breathing, or lethargy are red flags. Don’t wait longer. The infection might need a different antibiotic, or it could be something else entirely.
Are there alternatives to antibiotics for ear infections?
Yes. For many children over 6 months with mild ear infections, doctors recommend pain relief and observation for 48 to 72 hours. Studies show most ear infections clear up on their own. Pain relief with acetaminophen or ibuprofen, warm compresses, and rest are often enough. Antibiotics are only needed if symptoms persist or worsen.
Can antibiotics cause long-term gut problems in kids?
A single course of antibiotics rarely causes long-term issues. But repeated or unnecessary use can disrupt the gut microbiome, which plays a role in immunity, digestion, and even mood. Some studies link early, frequent antibiotic use to higher risks of asthma, allergies, and obesity later in life. That’s why it’s so important to use them only when truly needed.
Why do some doctors still prescribe antibiotics for colds?
Some do because parents ask for them - or because it’s easier than explaining why they’re not needed. But guidelines are clear: colds are viral. Antibiotics don’t help. Many clinics now use tools like CRP tests and delayed prescriptions to reduce pressure. If your doctor prescribes one for a cold, ask: “What’s the evidence this is bacterial?”
Jennifer Patrician
December 5, 2025 AT 07:19Antibiotics are just a gateway drug for Big Pharma to hook your kid on lifelong meds. They’re secretly adding fluoride and microchips to the syrup. I know a mom whose kid started talking in binary after amoxicillin. The CDC? Controlled by Monsanto. You think they care about your child? They want you dependent. Watch the documentary Antibiotic Apocalypse - it’s all connected to 5G and the vaccine agenda.
Mellissa Landrum
December 5, 2025 AT 16:25lol u think ur smart with ur ‘strep test’ bs? my niece got a rash after penicillin and now she cant eat dairy or breathe or whatever. they just wanna sell more drugs. i gave her honey and salt water and she was fine in 2 days. doctors are all just profit robots. #antibioticfreelife
Rupa DasGupta
December 5, 2025 AT 19:32My baby had a fever for 5 days and I didn't give any meds... just coconut oil on her feet and whispered affirmations. She smiled on day 4. The doctor said 'it's viral' but I knew it was her soul releasing toxins. 🌿💔 Antibiotics? No thank you. I'm not letting Big Pharma steal her energy. She's now 8 and never had a cold since. #NaturalHealing #TrustYourIntuition
Marvin Gordon
December 7, 2025 AT 19:00Really solid breakdown. I used to panic every time my kid had a fever, but after reading this, I’ve learned to wait. We’ve done the 48-hour watch for ear infections twice now - both times cleared up on their own. Honestly, it’s scary how much fear-based medicine there is out there. Glad more docs are using CRP now. Knowledge is power.
ashlie perry
December 7, 2025 AT 20:27Michael Dioso
December 8, 2025 AT 17:10Oh please. You think this is about science? The CDC’s 30% unnecessary prescription stat is cooked. They’re ignoring the fact that in 40% of cases, parents are pressured by daycare centers to medicate or keep the kid home. And let’s not forget - pediatricians get paid more for prescribing. It’s not ignorance. It’s economics. You’re being played.
Philip Kristy Wijaya
December 8, 2025 AT 19:54One must consider the broader epidemiological implications of antimicrobial stewardship in pediatric populations wherein the indiscriminate administration of beta-lactam antibiotics contributes to the selection pressure driving the evolution of multidrug resistant phenotypes within commensal flora thereby compromising the long term microbiological homeostasis of the host organism
Mark Curry
December 10, 2025 AT 04:04My daughter had a rash after amoxicillin too. We got her tested last year - turns out she’s not allergic. We gave her penicillin again for a bad ear infection and she was fine. Best decision we ever made. Don’t assume. Test. It’s simple. And it saves your kid from stronger meds later. 🤝