Anticholinergic Burden in Older Adults: How Common Medications Raise Dementia Risk

Many older adults take medications every day to manage pain, allergies, bladder issues, or depression. But what if some of those pills are quietly harming their brains? The truth is, a growing body of research shows that anticholinergic burden-the combined effect of multiple drugs that block acetylcholine-is one of the most preventable causes of cognitive decline in seniors. And it’s happening far more often than most people realize.
What Is Anticholinergic Burden?
Anticholinergic burden refers to the total impact of medications that block acetylcholine, a key chemical in the brain that helps with memory, attention, and learning. These drugs don’t just affect the body-they cross into the brain and interfere with brain circuits that control thinking. The more of these drugs someone takes, and the longer they take them, the greater the risk. There are three main scales doctors use to measure this burden: the Anticholinergic Cognitive Burden (ACB) scale, the Anticholinergic Risk Scale (ARS), and the Drug Burden Index (DBI). The ACB scale is the most widely used today. It rates each medication from Level 1 (mild) to Level 3 (strong). A person taking two Level 2 drugs and one Level 3 drug might have an ACB score of 7. That’s considered high. And high scores are linked to real brain changes.How These Drugs Damage the Brain
Acetylcholine is especially important in three brain areas: the hippocampus (memory), the cerebral cortex (thinking), and the neostriatum (movement and planning). When anticholinergics block these receptors, brain cells can’t communicate properly. Over time, this leads to measurable damage. A 2016 study in JAMA Neurology found that older adults taking even moderate amounts of these drugs had a 4% drop in glucose metabolism in brain regions affected by Alzheimer’s. That’s the same area that lights up in scans of people with early dementia. Another study tracked 451 seniors over three years and found those on anticholinergics lost brain volume 0.24% faster per year than those who weren’t. That may sound small, but over five years, it adds up to a noticeable difference in thinking ability. These aren’t just lab findings. Brain imaging studies show that the longer someone takes these drugs, the more their brain activity slows down. In one large trial of nearly 20,000 people over 70, those with higher ACB scores had worse scores on memory and word-finding tests every year-even if they started out cognitively normal.Which Medications Carry the Highest Risk?
Not all anticholinergics are the same. Some are stronger than others. The most common culprits in older adults include:- First-generation antihistamines: Diphenhydramine (Benadryl, Tylenol PM, Advil PM) - used for allergies or sleep. This is the #1 source of high ACB scores.
- Overactive bladder drugs: Oxybutynin (Ditropan), tolterodine, solifenacin - prescribed to reduce frequent urination.
- Tricyclic antidepressants: Amitriptyline, nortriptyline - older antidepressants still used despite newer, safer options.
- Some anti-nausea and motion sickness drugs: Dimenhydrinate (Dramamine), promethazine.
- Antipsychotics: Chlorpromazine, quetiapine - sometimes used off-label for sleep or agitation in dementia.
Cognitive Effects: What Gets Worse?
The damage isn’t random. Anticholinergics hit certain brain functions harder than others.- Executive function - planning, organizing, switching tasks - drops the most. In the ASPREE study, each point increase in ACB score led to a 0.15-point annual decline on word association tests.
- Episodic memory - remembering recent events or conversations - also declines significantly. Each ACB point meant a 0.08-point drop per year on memory recall tests.
- Processing speed - how fast someone thinks or reacts - shows the weakest link. Some studies found no real effect.

Long-Term Use = Higher Dementia Risk
It’s not just about feeling foggy today. The real danger is what happens over years. A landmark 2015 study from the University of Washington tracked over 3,400 seniors for more than a decade. Those who took anticholinergics for three years or more had a 54% higher chance of developing dementia than those who used them for less than three months. Even after adjusting for other health conditions, the link held strong. The American Geriatrics Society’s 2023 Beers Criteria now explicitly says: Avoid strong anticholinergics in older adults. They list diphenhydramine, oxybutynin, and amitriptyline as drugs that should be replaced if possible. And it’s not just observational data. In the DICE trial, 286 older adults with high ACB scores had their medications carefully reviewed and reduced. After 12 weeks, their Mini-Mental State Exam (MMSE) scores improved by 0.82 points on average. That’s a measurable jump in thinking ability-enough to help someone remember to take their pills or find their way home.Real Stories: When Stopping the Drug Changed Everything
Behind the numbers are real people. On AgingCare.com, a caregiver named Jen wrote: “My mom was confused all the time. She’d forget where she put her keys, get lost in her own house. We thought it was early dementia. Then we found out she’d been on oxybutynin for two years. We stopped it. Two weeks later, she was back to herself. Her doctor didn’t even know it could cause this.” The FDA’s adverse event database recorded over 1,200 cases of confusion, memory loss, or delirium linked to anticholinergics in seniors between 2018 and 2022. Most of these cases happened with drugs that were never labeled as “cognitive risks.” A 2021 survey by the National Council on Aging found that 63% of older adults were never told about these risks when their prescriptions were written. And 41% said they’d have chosen a different treatment if they’d known.Why Do Doctors Keep Prescribing Them?
It’s not that doctors don’t know. They do. But there are barriers. First, many of these drugs are cheap, widely available, and easy to prescribe. Oxybutynin treats overactive bladder quickly. Diphenhydramine helps with sleep. Amitriptyline helps with nerve pain. And for many doctors, it’s the first option they reach for. Second, switching isn’t simple. Replacing a drug means finding an alternative that works just as well. For bladder issues, mirabegron (Myrbetriq) is a non-anticholinergic option. For depression, SSRIs like sertraline or citalopram have far less brain impact. For allergies, loratadine (Claritin) or cetirizine (Zyrtec) are safer. Third, time is tight. A 2021 survey of over 1,200 family doctors found that reviewing all medications for anticholinergic risk takes an average of 23 minutes per patient. Most appointments are 15 minutes. Only 37% of doctors felt they had enough time to do it right. Even when high-risk prescriptions are flagged, they’re rarely acted on. One study found that only 39% of nursing home residents with high ACB scores had their meds reviewed within three months of being identified.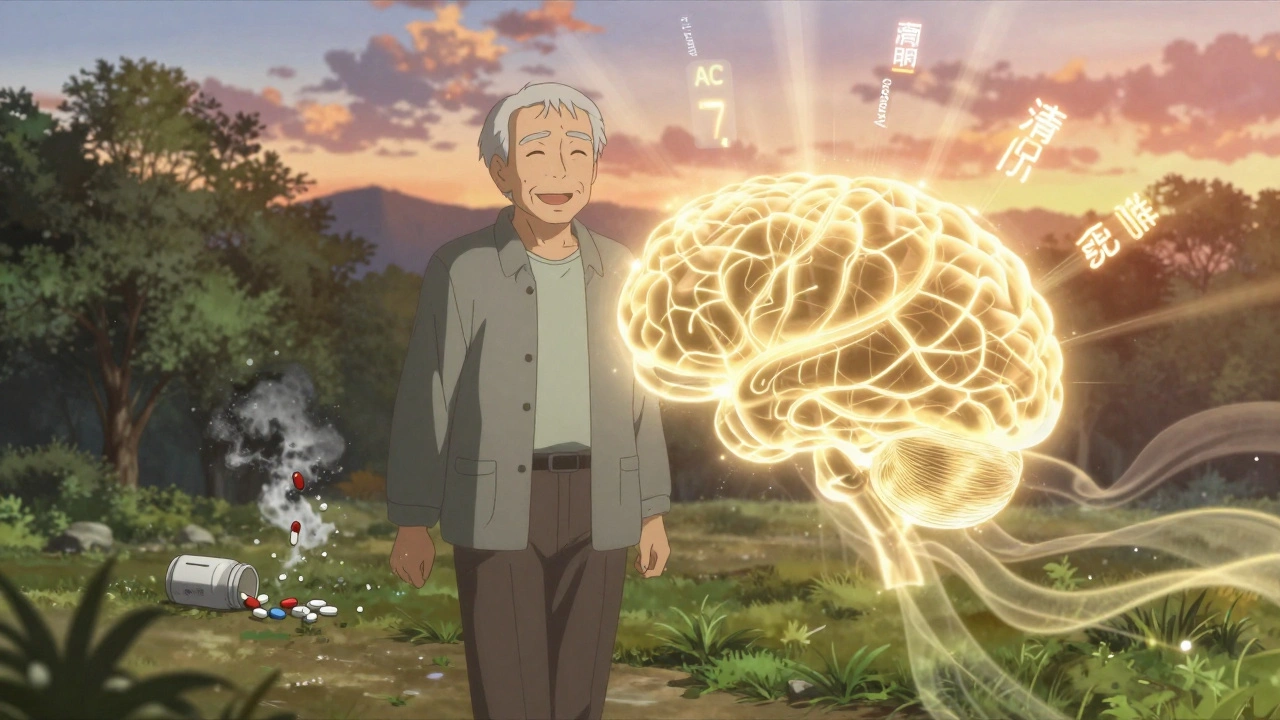
What Can You Do?
If you or a loved one is over 65 and taking any of these medications, here’s what to do:- Make a full list of every pill, patch, cream, or supplement you take-even over-the-counter ones.
- Check the ACB scale - the American Geriatrics Society now has a free mobile app called the ACB Calculator. Just enter the drug names and it gives you a score.
- Ask your doctor: “Is this drug anticholinergic? Is there a safer alternative?” Don’t be afraid to say, “I’ve read this might affect my memory.”
- Don’t stop cold - some drugs need to be tapered. Ask for a plan.
- Give it time - cognitive improvement can take 4 to 8 weeks after stopping. Be patient.
The Bigger Picture
The Lancet Healthy Longevity Commission named anticholinergic burden one of the top 10 modifiable risk factors for dementia-possibly contributing to 10-15% of cases. That’s like removing smoking or high blood pressure from the list of dementia causes. Pharmaceutical companies are starting to respond. Johnson & Johnson stopped making long-acting oxybutynin in 2021. Pfizer pushed solifenacin, which is safer for the brain. The FDA now requires updated warning labels on all anticholinergic drugs. And the National Institute on Aging is funding a $14.7 million study to see if reducing these drugs can actually delay dementia. But until that research is complete, the best tool we have is awareness. The brain changes caused by these drugs aren’t inevitable. They’re reversible. And they’re preventable.When to Get Help
If you notice any of these signs in an older adult:- Sudden confusion or disorientation
- Forgetting recent conversations or appointments
- Difficulty following instructions
- Slowed thinking or speech
- Increased falls or clumsiness
What is anticholinergic burden?
Anticholinergic burden is the combined effect of medications that block acetylcholine, a brain chemical critical for memory and thinking. It’s measured using scales like the ACB scale, which rates drugs from mild to strong. The more drugs you take and the stronger they are, the higher your burden-and the greater your risk of cognitive decline.
Which common over-the-counter drugs have anticholinergic effects?
Diphenhydramine (found in Benadryl, Tylenol PM, Advil PM) is the most common. Other OTC options include dimenhydrinate (Dramamine) and some sleep aids with hidden antihistamines. Even though they’re available without a prescription, they can significantly raise anticholinergic burden in older adults.
Can stopping anticholinergic drugs improve memory?
Yes. Studies show that when older adults stop taking high-anticholinergic drugs, cognitive function often improves within 4 to 8 weeks. In one trial, participants saw measurable gains in memory and thinking tests after 12 weeks of deprescribing. The brain can recover, especially if the drugs were taken for less than a few years.
Are there safer alternatives to anticholinergic medications?
Absolutely. For allergies, use loratadine or cetirizine instead of diphenhydramine. For overactive bladder, mirabegron is a non-anticholinergic option. For depression, SSRIs like sertraline are much safer for the brain than amitriptyline. For sleep, cognitive behavioral therapy (CBT-I) is more effective long-term than sleep aids.
How can I check my anticholinergic burden?
The American Geriatrics Society offers a free mobile app called the ACB Calculator. Just enter your medications, and it gives you a score based on the latest ACB scale. You can also ask your pharmacist or doctor to review your list using the ACB scale. A score of 3 or higher is considered high risk.
Is anticholinergic burden linked to Alzheimer’s disease?
It’s not Alzheimer’s itself, but it mimics its early signs and may speed up its development. Brain scans show reduced activity in the same areas affected by Alzheimer’s. Long-term use increases dementia risk by over 50%. Reducing anticholinergic burden may delay or even prevent dementia in some people.
Why aren’t doctors more aware of this risk?
Many doctors know, but time constraints make it hard to review all medications. A full review takes about 23 minutes per patient-longer than most appointments. Also, some anticholinergics are prescribed for conditions with no obvious alternatives, and older doctors may have been trained to see them as safe. Awareness is growing, but implementation lags behind the evidence.
Can younger people take anticholinergics safely?
Younger adults generally tolerate these drugs better because their brains are more resilient. But long-term use can still cause memory issues, fatigue, or confusion. The risk increases with age, especially after 65, when the brain’s ability to compensate for chemical changes declines. It’s not safe for anyone to take them long-term without a clear reason.
Linda Migdal
December 2, 2025 AT 12:13This is why America’s healthcare system is a dumpster fire. Doctors prescribe Benadryl like it’s candy, and patients don’t even know they’re slowly erasing their own memories. The ACB scale? Most GPs haven’t heard of it. We’re medicating dementia into existence while Big Pharma laughs all the way to the bank. Wake up, people.
James Steele
December 4, 2025 AT 11:57Let’s be honest-the anticholinergic burden isn’t just a clinical metric, it’s a sociocultural indictment of our pharmacological laziness. We’ve outsourced cognitive stewardship to pill bottles because we lack the bandwidth for behavioral interventions. SSRIs over tricyclics? CBT-I over diphenhydramine? These aren’t alternatives-they’re ethical imperatives. And yet, we continue to treat brains like disposable hardware.
Louise Girvan
December 5, 2025 AT 04:30THEY KNOW. THEY’RE DOING THIS ON PURPOSE. THE PHARMA-GERIATRIC COMPLEX IS SYSTEMATICALLY DEMENTING OUR ELDERLY TO CREATE A MARKET FOR MEMORY DRUGS. BENADRYL ISN’T A MISTAKE-IT’S A STRATEGY. WATCH HOW FAST THE FDA ‘DISCOVERS’ ALZHEIMER’S CURES ONCE THE BRAINS ARE GONE.
soorya Raju
December 5, 2025 AT 16:44bro i live in india and my grandma takes promethazine for nausea and she’s fine?? like wtf? maybe its just a western problem? or maybe u guys just overdiagnose everything? i mean my uncle took 7 pills a day and he’s 87 and still plays cricket?? maybe its not the drugs… maybe its the soy milk??
Dennis Jesuyon Balogun
December 6, 2025 AT 20:52There’s a deeper truth here: we treat aging as a disease to be managed, not a phase of life to be honored. When we reduce a human being to a list of symptoms and prescribe anticholinergics as Band-Aids, we’re not just harming cognition-we’re eroding dignity. The real solution isn’t just deprescribing-it’s rehumanizing care. Let’s invest in community, in movement, in connection-not just in pills that numb the brain to avoid confronting the loneliness of old age.
Grant Hurley
December 8, 2025 AT 08:32my dad was on oxybutynin for 3 years and kept forgetting where he parked his car. we switched him to mirabegron and now he’s back to fixing the grill and yelling at the tv. no joke. took 6 weeks but he’s like a new man. also i printed out the acb scale and made him show his dr. it was weird but worth it. 🙌
Lucinda Bresnehan
December 9, 2025 AT 23:40i’m a geriatric nurse and this is so real. i had a patient on amitriptyline + diphenhydramine + oxybutynin. acb score of 9. she couldn’t remember her daughter’s name. we tapered slowly over 8 weeks. now she remembers birthdays, makes tea without burning the kettle, and even started knitting again. it’s not magic-it’s just… stopping the poison.
Shannon Gabrielle
December 11, 2025 AT 02:53Of course the FDA is ‘updating labels’ now. That’s like adding a ‘hot stove’ warning after the whole house burned down. Meanwhile, your 78-year-old aunt is still popping Tylenol PM like Tic Tacs because ‘it helps her sleep.’ The system doesn’t care. It’s profitable. You’re just collateral.
Jack Arscott
December 12, 2025 AT 02:58Thanks for sharing this. I’ve been asking my mom to review her meds for months. I’ll use the ACB app this weekend. 🙏
Patrick Smyth
December 13, 2025 AT 21:05It is a tragedy. A profound, systemic tragedy. I have watched my father-once a brilliant engineer-become a ghost in his own home, all because of a simple bladder pill. The medical establishment has failed us. Not through malice, but through indifference. And indifference is the most dangerous drug of all.
Declan O Reilly
December 14, 2025 AT 07:25wait so if i stop my benadryl will i stop forgetting where i put my keys? i mean i’ve been taking it for 10 years but i also drink 3 coffees a day and watch netflix till 3am… is it the pills or my life choices? 🤔
Conor Forde
December 14, 2025 AT 08:57Here’s the real conspiracy: the ‘ACB scale’ was invented by a pharmaceutical consultant who used to work for Pfizer. Coincidence? I think not. They need you to think the problem is ‘too many drugs’ so they can sell you the ‘safer’ version… for $200 a month. The real solution? Stop taking all pills. Go live in a cabin. Eat mushrooms. Meditate. The brain heals when you stop poisoning it-with drugs, with screens, with capitalism.