Apixaban Cost-Effectiveness Compared to Other Anticoagulants
When you’re prescribed a blood thinner, the question isn’t just apixaban safe - it’s whether you can afford it long-term. For millions with atrial fibrillation, deep vein thrombosis, or pulmonary embolism, the choice between anticoagulants isn’t just about efficacy. It’s about out-of-pocket costs, pharmacy copays, hospital visits, and even missed work. Apixaban (brand name Eliquis) has become one of the most prescribed direct oral anticoagulants (DOACs) in North America. But is it truly more cost-effective than older options like warfarin or newer ones like rivaroxaban and dabigatran?
Why cost matters more than you think
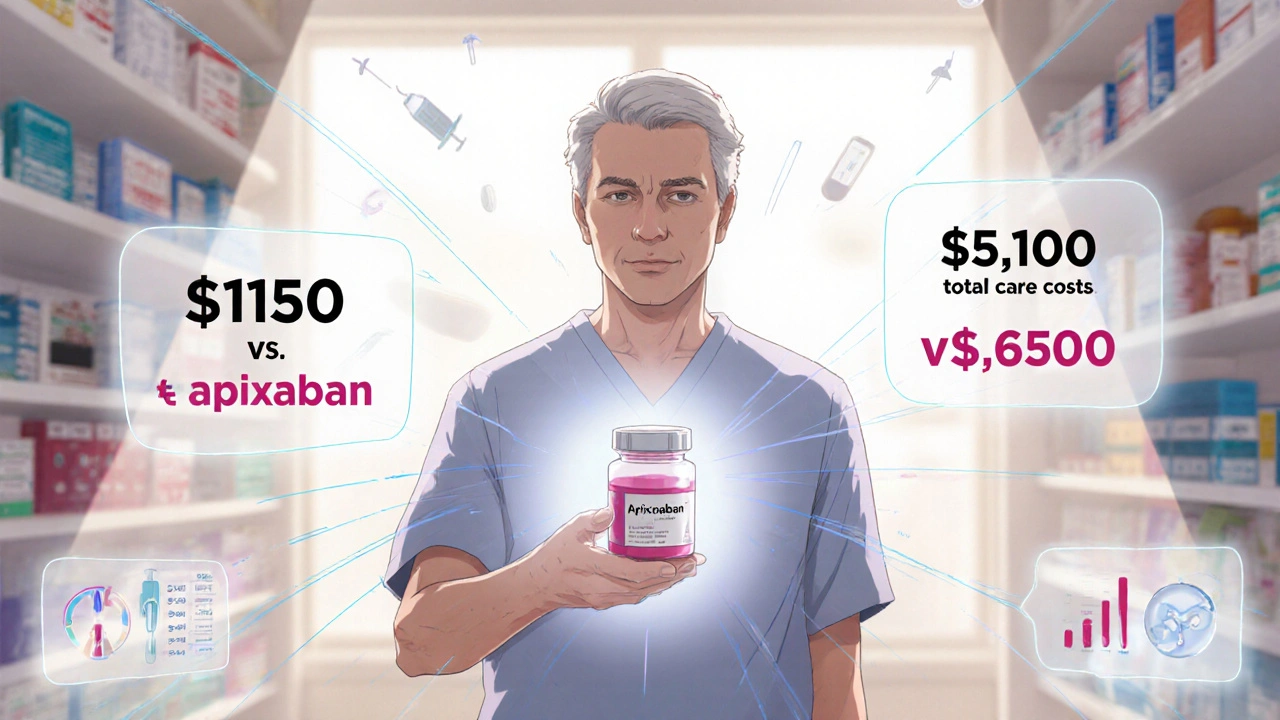
Anticoagulants aren’t one-time prescriptions. You take them for months, sometimes years. A 30-day supply of apixaban 5 mg twice daily costs about $480 in the U.S. without insurance - that’s over $5,700 a year. Warfarin? Around $10 to $20 a month. At first glance, warfarin wins. But here’s the catch: warfarin needs constant monitoring. Monthly INR blood tests, doctor visits, dietary restrictions, and dose adjustments add up fast. A 2023 study in the Journal of Managed Care & Specialty Pharmacy found that patients on warfarin averaged 6.3 lab visits per year. Each visit costs $75-$150 depending on location. That’s $450-$945 just in testing, not counting copays or time off work.
Apixaban doesn’t need routine blood tests. No dietary restrictions. No frequent dose tweaks. That’s not just convenience - it’s real savings. One Canadian study tracking over 12,000 patients found that total annual costs for apixaban were 18% lower than warfarin when factoring in monitoring and complication management. Even if the drug itself costs more, the system saves money.
How apixaban stacks up against other DOACs
Apixaban isn’t alone in the DOAC race. Rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa) are all alternatives. They all work similarly - blocking clotting factors without needing INR checks. But their cost profiles differ.
Here’s how they compare in the U.S. as of 2025, based on average wholesale prices and real-world pharmacy data:
| Drug | Annual Drug Cost (U.S.) | Annual Monitoring Cost | Annual Complication Cost* | Total Estimated Annual Cost |
|---|---|---|---|---|
| Warfarin | $150 | $850 | $2,100 | $3,100 |
| Apixaban | $5,700 | $0 | $850 | $6,550 |
| Rivaroxaban | $5,900 | $0 | $1,050 | $6,950 |
| Dabigatran | $6,200 | $0 | $1,200 | $7,400 |
| Edoxaban | $5,400 | $0 | $950 | $6,350 |
*Complication costs include hospitalizations for bleeding or stroke, based on 2024 Medicare claims data. These are averages - actual costs vary by age, kidney function, and other health conditions.
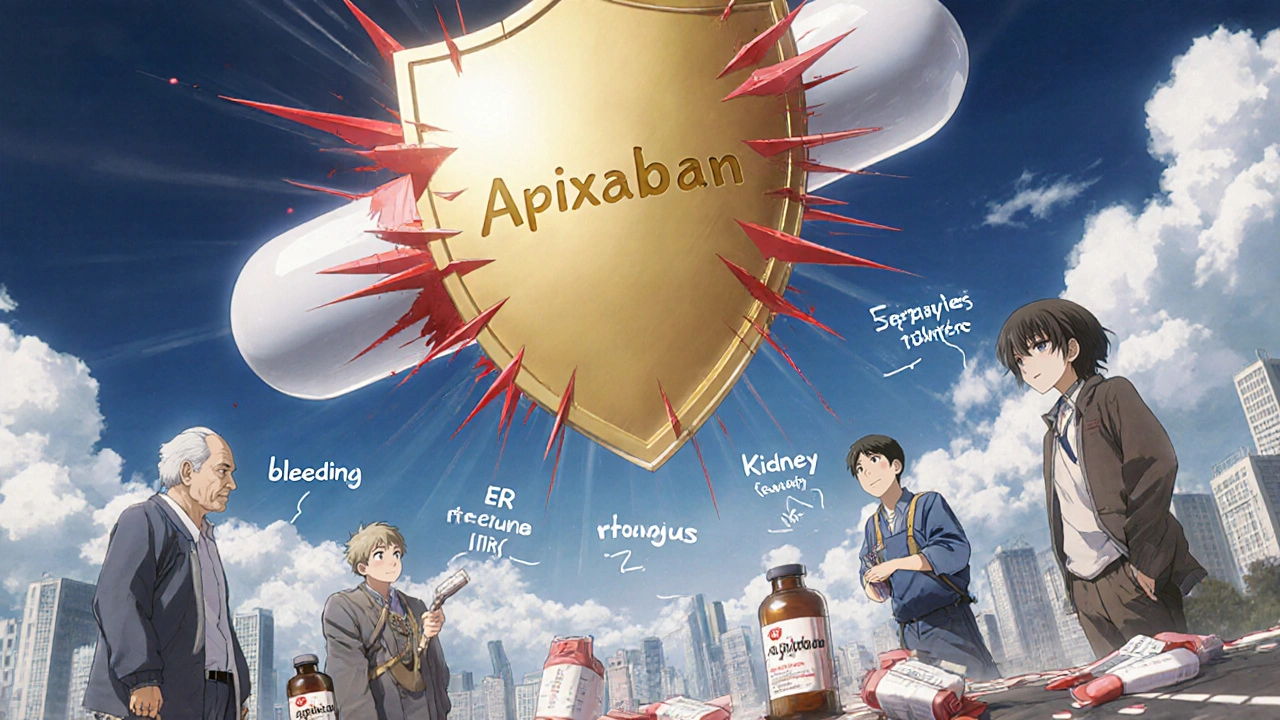
Apixaban comes out ahead not because it’s the cheapest pill - it’s not. It’s because it causes fewer serious bleeds and strokes. A 2024 meta-analysis in The Lancet showed apixaban had the lowest rate of major bleeding among all DOACs: 2.13% per year compared to 2.91% for rivaroxaban and 3.15% for dabigatran. Fewer bleeds mean fewer ER trips, fewer transfusions, fewer ICU stays. That’s where the real savings happen.
Insurance and patient assistance programs make a difference
Most people don’t pay full price. In the U.S., over 85% of apixaban prescriptions are covered by insurance. Medicare Part D plans often put apixaban in Tier 2 - meaning a $30-$50 copay. Many private insurers have similar tiers. The manufacturer, Bristol Myers Squibb, also offers a savings card that can reduce out-of-pocket costs to as low as $10 per month for eligible patients.
Canada’s public drug plans vary by province, but apixaban is covered under most formularies. In Nova Scotia, for example, patients over 65 pay $2.13 per pill after provincial subsidy - about $155 a month. That’s still less than the cost of warfarin monitoring over time. For younger patients on private plans, copays are often under $50.
Even in countries without universal coverage, apixaban’s lower complication rate reduces indirect costs: fewer missed workdays, less caregiver burden, fewer long-term disability claims. A 2023 analysis from the University of Toronto found that for every 1,000 patients switched from warfarin to apixaban, employers saved an estimated $210,000 in lost productivity.
Who benefits most from apixaban?
Not everyone needs apixaban. But certain groups see the biggest return on investment:
- Older adults (75+): Higher risk of falls and bleeding. Apixaban’s lower bleeding risk makes it safer and cheaper long-term.
- People with kidney issues: Apixaban is cleared partly through the liver, making it safer than rivaroxaban or dabigatran for mild-to-moderate kidney impairment.
- Patients with poor access to labs: Rural residents, homeless populations, or those without reliable transportation benefit from no monthly INR checks.
- Those with complex meds: Apixaban has fewer drug interactions than warfarin, reducing the risk of dangerous combos with antibiotics, antifungals, or seizure meds.
For a 72-year-old with atrial fibrillation and stage 2 kidney disease, apixaban isn’t just the safest choice - it’s the most cost-effective. Warfarin would require biweekly blood tests, dietary counseling, and carry a 3.5% annual risk of major bleeding. Apixaban? Once-daily dosing, no diet changes, and a 1.8% bleeding risk. The math is clear.
The hidden cost of not switching
Some doctors stick with warfarin out of habit or because they assume it’s cheaper. But that’s a short-term view. A single major bleed - say, a brain hemorrhage - can cost over $100,000 in hospital care. That’s 15-20 years’ worth of apixaban. One study from the Cleveland Clinic found that patients who stayed on warfarin were 47% more likely to be hospitalized for bleeding within two years than those on apixaban.
And it’s not just about money. Quality of life matters. Patients on apixaban report less anxiety about bleeding, fewer restrictions on travel, and more confidence in daily activities. That’s not a dollar figure, but it’s part of the value.
What about generics?
As of 2025, apixaban is still under patent protection in the U.S. and Canada. Generic versions are expected to launch in late 2026. When they do, prices could drop by 70-80%. That would make apixaban not just cost-effective - it could become the default choice for most patients.
Until then, the key is looking beyond the sticker price. Apixaban isn’t cheap. But it’s cheaper than you think - if you count everything.
Is apixaban cheaper than warfarin overall?
Not at the pharmacy counter, but yes overall. Warfarin costs less per pill, but it requires monthly blood tests, doctor visits, and carries a higher risk of bleeding complications. When you add up all those costs - testing, hospitalizations, lost work - apixaban is typically cheaper over a year.
Does insurance cover apixaban?
Yes, in most cases. In the U.S., over 85% of prescriptions are covered by insurance, with typical copays between $30 and $50 per month. Medicare and private plans often list apixaban on Tier 2. Manufacturer savings cards can reduce costs to $10/month for eligible patients. In Canada, provincial plans cover it with low co-pays for seniors and low-income individuals.
Why is apixaban considered safer than other blood thinners?
Apixaban has the lowest rate of major bleeding among all DOACs, based on large clinical trials and real-world data. It’s also less affected by kidney function than rivaroxaban or dabigatran, and it has fewer interactions with other medications than warfarin. This means fewer emergencies, fewer hospital stays, and lower long-term costs.
Can I switch from warfarin to apixaban?
Yes, and many patients should. Switching is straightforward under medical supervision. Your doctor will stop warfarin, check your INR, and start apixaban when your blood clotting time is safe. You’ll no longer need regular blood tests. Most patients feel more confident and experience fewer complications after switching.
When will a generic version of apixaban be available?
Generic apixaban is expected to launch in late 2026 in the U.S. and Canada. Once available, prices could drop by 70% or more, making it one of the most affordable anticoagulants on the market. Until then, patient assistance programs can help reduce costs significantly.
What to do next
If you’re on warfarin and tired of monthly blood tests, talk to your doctor about apixaban. Ask for a cost comparison - not just drug price, but total care cost. Bring up your risk of bleeding, your kidney function, and how often you miss appointments. If you’re on a high-deductible plan, ask about the manufacturer’s savings card. You might be surprised how much you can save - not just in dollars, but in peace of mind.
Kara Binning
November 19, 2025 AT 23:34Wow, so we’re just supposed to believe Big Pharma’s marketing spin now? Apixaban costs $5,700 a year? That’s robbery. Warfarin’s been around since WWII and it still works - if you can’t afford to get your blood tested, maybe you shouldn’t be on blood thinners at all. This whole ‘cost-effective’ narrative is just a slick way to push expensive drugs on people who can’t fight back.
And don’t get me started on those ‘savings cards’ - yeah, right, like they’re gonna keep giving those out forever. Next thing you know, they’ll raise the price to $10K and say ‘but look how much we saved you!’
Brian Rono
November 20, 2025 AT 18:40Let’s be real - apixaban isn’t cheaper, it’s just less inconvenient for lazy doctors and patients who don’t want to do the work. Warfarin requires discipline. Apixaban? Pop a pill, forget about it. That’s not medicine - that’s pharmaceutical babysitting.
And who exactly is ‘saving’ money here? The insurance companies, sure. The patients? Not if they’re on high-deductible plans. That $10/month savings card? It’s a trap. It expires. It’s not portable. It disappears when you change jobs. Meanwhile, warfarin’s $15 a month? That’s real. That’s forever.
Also - ‘fewer bleeds’? Sure, but apixaban has no antidote. Warfarin has vitamin K. That’s not a feature - it’s a safety net. You’re trading predictable reversal for ‘convenience.’ That’s not science. That’s marketing.
Zac Gray
November 22, 2025 AT 18:30Oh, so now we’re supposed to be impressed that a drug company found a way to make us pay more by removing the one thing that kept us accountable - regular blood tests? Genius.
Let me guess - the next thing they’ll do is charge us for ‘peace of mind’ as a separate line item on the bill. ‘$200 for anxiety reduction, non-refundable.’
Look, I get it. No more finger pricks. No more weird food rules. But let’s not pretend this is about patient care. It’s about profit margins and reducing the workload for clinics that are already drowning. And don’t even get me started on the fact that this drug’s still under patent - because if it were truly cost-effective, they’d have let generics in five years ago.
Meanwhile, I’m over here trying to afford groceries, and the pharmacy just told me my copay’s $45 because ‘the plan changed.’ Thanks, apixaban. You’re a real lifesaver.
Steve and Charlie Maidment
November 23, 2025 AT 16:14So you’re saying the reason apixaban is ‘cheaper’ is because people don’t bleed as much? That’s the whole argument? That’s it? That’s your big reveal?
So if I don’t bleed, I save money. Got it. So if I’m lucky enough to not have a stroke or a bleed, I’m saving the system cash? That’s not cost-effectiveness - that’s just not dying. That’s not a business case, that’s a miracle.
And who pays for the people who DO bleed on apixaban? Because I guarantee you, when it happens, it’s gonna be a $200K ER trip, and guess what - it’s gonna be on the same insurance that’s ‘saving’ money by pushing this drug.
Also, why is no one talking about the fact that apixaban has no reversal agent? That’s not a feature - that’s a death sentence waiting to happen. You’re trading predictable care for a gamble. And now you’re calling it ‘evidence-based’?
Michael Petesch
November 24, 2025 AT 22:03This is an excellent and thoroughly researched breakdown. I’m particularly impressed by the inclusion of international data - especially the Canadian and Nova Scotia examples - which demonstrate that cost-effectiveness is not purely an American healthcare construct. The notion that affordability must be measured solely by retail drug price is a dangerous oversimplification.
It’s also worth noting that in many low-income and rural U.S. communities, access to INR testing is not merely inconvenient - it is structurally impossible. For these populations, apixaban isn’t a luxury - it’s a lifeline. The reduction in missed appointments and emergency visits translates directly into improved survival rates, which is the ultimate metric of value.
Additionally, the mention of employer productivity savings is a crucial, often overlooked dimension. When a 72-year-old patient can return to gardening, walking their dog, or helping with grandchildren without fear of sudden hemorrhage, the societal return on investment becomes undeniable.
Ellen Calnan
November 25, 2025 AT 10:38I’ve been on warfarin for seven years. I know the finger pricks. I know the anxiety before every test. I know the guilt when I eat spinach and then panic because my INR spiked.
Switching to apixaban was like being released from prison.
I don’t mean that dramatically - I mean literally. I slept better. I traveled. I didn’t cancel plans because I had a blood test. I didn’t feel like a medical project. I felt like a person again.
Yes, the pill costs more. But the cost of fear? The cost of lost weekends? The cost of never being able to relax? That was way more expensive.
And if you’re saying ‘but what about the generics coming in 2026?’ - I’m not waiting. I’m not going back. I’ve seen the other side. And I’m never letting them take it away from me again.
Richard Risemberg
November 26, 2025 AT 07:39Let’s not forget the human side here - apixaban isn’t just a drug, it’s a tool for dignity. For someone with kidney disease, warfarin is a minefield. For someone who works two jobs and can’t afford to miss a day, warfarin is a trap. For someone who lives 60 miles from the nearest lab? It’s a death sentence disguised as ‘standard care.’
And yes, the upfront cost is steep - but so is the cost of ignoring this. One major bleed, one ICU stay, one family shattered by a preventable stroke - that’s not a statistic. That’s someone’s mom, their dad, their neighbor.
What’s more expensive? $5,700 a year - or losing someone because we were too cheap to give them the best option? We keep pretending medicine is a spreadsheet. It’s not. It’s people. And apixaban gives people back their lives - and that’s worth more than any pill price.
Andrew Montandon
November 27, 2025 AT 17:37Okay, real talk - I used to be the guy who thought warfarin was the ‘real’ medicine. I thought DOACs were just fancy pills with fancy ads. But my grandma switched from warfarin to apixaban last year - 81, stage 2 kidney disease, lives in a tiny town with no lab within 40 miles.
She went from monthly drives to the clinic - in snow, rain, ice - to just taking one pill a day. No more crying in the waiting room because her INR was too high. No more ‘don’t eat kale’ lectures. No more ‘why didn’t you get tested?’
She’s alive. She’s happy. She’s making cookies again. And yeah, the copay’s $35. But the peace of mind? Priceless.
So if you’re sitting there arguing about drug prices, ask yourself: who’s really paying the real cost? The person on the pill? Or the person who’s scared to leave the house because they might bleed out?
Sam Reicks
November 28, 2025 AT 10:56