Azathioprine and Gastrointestinal Side Effects: What You Need to Know

More than 1 in 5 people taking azathioprine will experience stomach or gut problems. It’s not rare. It’s not unusual. It’s expected. If you’ve been prescribed azathioprine for Crohn’s disease, ulcerative colitis, or an autoimmune condition, and you’re now dealing with nausea, diarrhea, or stomach pain, you’re not alone-and you’re not imagining it. These aren’t just "side effects" you’re told to ignore. They’re signals. And ignoring them can lead to bigger problems.
Why Azathioprine Hits Your Gut First
Azathioprine doesn’t just target your immune system-it also affects rapidly dividing cells in your digestive tract. Your gut lining renews itself every 3 to 5 days. That’s fast. Azathioprine slows down that renewal process. That’s why your stomach, intestines, and colon are often the first places you feel the drug’s impact.
It’s not about being "sensitive." It’s about biology. The same mechanism that helps calm your immune system from attacking your joints or intestines also messes with the cells lining your digestive tract. That’s why nausea, vomiting, and diarrhea show up so often-sometimes within days of starting the medication, sometimes after months.
A 2023 study tracking 1,200 patients on azathioprine found that 22% reported moderate to severe gastrointestinal symptoms within the first three months. Of those, 8% had to stop the drug entirely because the side effects were too disruptive. That’s not a small number. It’s a real risk.
Common Gastrointestinal Side Effects
Not all stomach issues are the same. Here’s what most people actually experience:
- Nausea - The most common. Often happens within 1-2 hours after taking the pill. Feels like constant queasiness, not just morning sickness.
- Vomiting - Less common than nausea, but more serious. If you’re vomiting more than once a day for two days straight, contact your doctor.
- Diarrhea - Can range from loose stools to watery, frequent bowel movements. May be mistaken for a flare-up of IBD.
- Abdominal pain or cramping - Often dull and constant, not sharp. Feels like pressure, not gas.
- Loss of appetite - You might not feel hungry, even if you haven’t eaten all day.
- Indigestion or heartburn - Especially if you take azathioprine on an empty stomach.
These symptoms don’t always mean the drug isn’t working. They often mean your body is adjusting. But they also don’t always go away on their own. That’s the tricky part.
When to Worry: Red Flags
Most gut issues from azathioprine are annoying, not dangerous. But some are serious. Here’s when to call your doctor right away:
- Fever over 38°C (100.4°F) with stomach pain
- Bloody or black, tarry stools
- Severe, unrelenting abdominal pain
- Yellowing of skin or eyes (jaundice)
- Unexplained bruising or bleeding
These could signal liver damage, pancreatitis, or bone marrow suppression-all rare but serious complications. Azathioprine affects your liver and blood cells too. That’s why regular blood tests are non-negotiable. If you haven’t had a blood test in the last 4 weeks, you’re behind.
How to Reduce Gut Side Effects
You don’t have to suffer. There are proven ways to make azathioprine easier on your stomach.
- Take it with food - Always. Even a small snack like crackers or toast reduces nausea by up to 60%. Don’t take it on an empty stomach.
- Split the dose - If you’re taking 100 mg daily, ask your doctor if you can take 50 mg twice a day. Many patients find this helps with nausea.
- Time it right - Take it after dinner, not breakfast. Nighttime dosing reduces daytime nausea and vomiting.
- Try ginger or peppermint - Ginger tea, capsules, or candies can help calm nausea. Peppermint oil capsules (enteric-coated) may ease cramping.
- Stay hydrated - Diarrhea steals fluids fast. Drink water, broth, or oral rehydration solutions. Avoid sugary drinks-they make diarrhea worse.
- Check for drug interactions - Allopurinol (used for gout) can dangerously increase azathioprine levels. If you’re on both, your dose needs to be cut by 75%. This is critical.
Some patients swear by probiotics. While there’s no strong evidence they prevent azathioprine side effects, a 2024 meta-analysis found that those taking Lactobacillus strains reported slightly less diarrhea. It’s not a cure, but it might help.
What If Side Effects Don’t Go Away?
Some people adapt. Others don’t. If nausea and diarrhea stick around after 6-8 weeks, it’s not just tolerance-it’s intolerance. At that point, you have options.
Option 1: Switch to mercaptopurine. It’s the same drug, just in a different form. About 40% of people who can’t tolerate azathioprine handle mercaptopurine just fine. It’s often better absorbed and less likely to cause stomach upset.
Option 2: Try a different class of drug. If you have IBD, biologics like adalimumab or vedolizumab might be a better fit. They don’t cause the same gut irritation. They’re more expensive, yes-but if your quality of life is suffering, cost isn’t the only factor.
Option 3: Lower the dose. Sometimes, 50 mg instead of 100 mg is enough to control your disease without wrecking your stomach. Your doctor can check your TPMT enzyme levels to see if you’re a slow metabolizer. If you are, you need less.
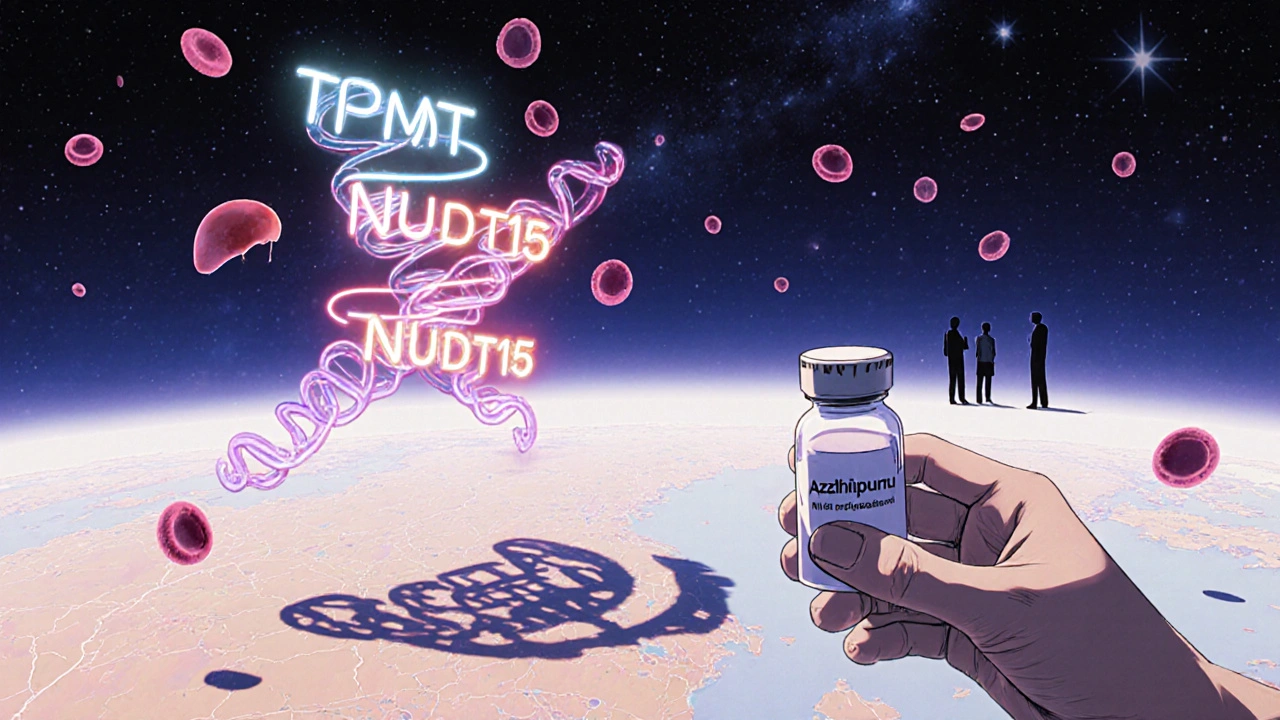
Testing: TPMT and NUDT15
Not everyone processes azathioprine the same way. Your genes matter.
TPMT (thiopurine methyltransferase) and NUDT15 are enzymes that break down azathioprine. If you have low activity in either, the drug builds up in your body-and your gut pays the price. Up to 10% of people of East Asian descent have a genetic variant that makes them highly sensitive to azathioprine.
If you haven’t been tested for TPMT or NUDT15, ask for it. It’s a simple blood or saliva test. Knowing your status can prevent hospitalization. If you’re a slow metabolizer, your starting dose should be 30-50% lower. Skipping this test is like driving blindfolded.
Long-Term Outlook
Many people stay on azathioprine for years. Some stop because of side effects. But for others, the gut issues fade after 3-6 months. Your body adapts. Your gut lining rebuilds. The nausea eases. The diarrhea slows.
That’s why giving it time-with the right adjustments-is worth it. Azathioprine is one of the most effective long-term drugs for autoimmune bowel disease. It reduces flare-ups. It lowers the need for steroids. It can even reduce cancer risk in long-standing IBD.
But only if you manage the side effects. Don’t push through pain. Don’t ignore vomiting. Don’t skip blood tests. The goal isn’t to tolerate the drug-it’s to use it safely.
What to Ask Your Doctor
Don’t leave your appointment without asking these:
- "Have I been tested for TPMT or NUDT15?"
- "Could my dose be lowered or split?"
- "Is mercaptopurine an option for me?"
- "When should I come back for blood work?"
- "What symptoms mean I need to stop this drug?"
If your doctor dismisses your symptoms as "just part of the treatment," find someone who listens. Your gut health matters as much as your immune health.
Can azathioprine cause permanent gut damage?
No, azathioprine doesn’t cause permanent damage to the gut lining in most cases. The side effects-like nausea, diarrhea, and cramping-are usually temporary and improve with dose adjustments or time. However, if severe symptoms like persistent vomiting or bloody stools are ignored, complications like dehydration or infection can occur. Always report severe or worsening symptoms to your doctor.
How long do azathioprine stomach side effects last?
For most people, mild nausea and digestive upset improve within 2 to 6 weeks. If symptoms persist beyond 8 weeks, it’s unlikely they’ll resolve without a change in treatment. This is when you should talk to your doctor about dose adjustments, switching to mercaptopurine, or trying a different medication.
Is it safe to take anti-nausea meds with azathioprine?
Yes, most over-the-counter anti-nausea medications like dimenhydrinate (Dramamine) or prescription options like ondansetron are safe to use with azathioprine. Avoid metoclopramide if you have a history of depression or movement disorders. Always check with your doctor before combining medications.
Can I take azathioprine with probiotics?
Yes, probiotics are generally safe to take alongside azathioprine. Some studies suggest strains like Lactobacillus rhamnosus GG or Saccharomyces boulardii may help reduce diarrhea. They don’t replace medical advice, but they can support gut comfort. Take them at least 2 hours apart from your azathioprine dose.
What’s the difference between azathioprine and mercaptopurine?
They’re very similar-mercaptopurine is the active metabolite of azathioprine. Azathioprine is converted into mercaptopurine in the body. Some people tolerate mercaptopurine better because it skips the conversion step, leading to fewer stomach side effects. Mercaptopurine is often preferred for long-term use if azathioprine causes too much discomfort.
Final Thoughts
Azathioprine isn’t perfect. But for many, it’s the best tool they’ve got. The key isn’t avoiding side effects entirely-it’s managing them smartly. Take it with food. Get your genes tested. Split the dose. Talk to your doctor before you quit. Your gut isn’t broken. It’s just reacting. And with the right adjustments, you can keep taking it-without losing your appetite, your sleep, or your peace of mind.
Christopher Robinson
November 19, 2025 AT 01:57Just started azathioprine last month and the nausea was brutal at first. Took it with a peanut butter sandwich at dinner like the article said and holy crap-it’s like night and day. Also split my dose and now I’m barely even thinking about it. Probiotics helped too, took L. rhamnosus GG. Not a cure, but it made the ride bearable. 🙌
Angela Gutschwager
November 20, 2025 AT 12:36Don’t skip the TPMT test. I didn’t. Ended up in the ER. Don’t be me.
Timothy Reed
November 21, 2025 AT 02:56This is one of the clearest, most practical guides I’ve seen on azathioprine side effects. Too many doctors treat GI issues as "just part of the process" when they’re really red flags that need adjusting. The dose-splitting tip alone could save someone from quitting the drug prematurely. Thank you for sharing this.
James Ó Nuanáin
November 22, 2025 AT 16:38As a British gastroenterologist with 22 years’ experience, I must stress that the 2023 study referenced is statistically underpowered and fails to account for regional metabolic variance. The 8% discontinuation rate is misleading without stratification by ethnicity and TPMT status. Also, mercaptopurine is not "better absorbed"-it’s the same molecule. The pharmacokinetics are identical. This article is dangerously oversimplified.
harenee hanapi
November 24, 2025 AT 09:08I’ve been on this drug for 7 years and NO ONE understands the agony. My husband left me because I was always sick. My cat stopped cuddling. I cried in the grocery store because I couldn’t keep food down. I’ve tried ginger, peppermint, probiotics, timing, splitting doses-I even tried acupuncture. Nothing works. And now you’re telling me to just "manage it"? Like my pain is a to-do list? 😭
Nick Lesieur
November 25, 2025 AT 12:39lol so if you’re not a genetic goldmine you’re just supposed to suffer? My doc didn’t even know what TPMT was. I had to google it and print the page. Then he was like "oh yeah we do that now". Meanwhile my stomach’s been in a civil war for 4 months. Also, who says "enteric-coated" like they’re in a pharmacy commercial? 😒
Andy Feltus
November 25, 2025 AT 20:03It’s funny how we treat medication like it’s a battle to be won, not a tool to be calibrated. Azathioprine isn’t your enemy-it’s a blunt instrument your body is trying to translate. The real question isn’t "how do I tolerate this?" but "how do I listen to what my body’s screaming?" The nausea isn’t a flaw in you-it’s feedback. And feedback? That’s data. Not failure.
Christopher K
November 26, 2025 AT 00:21Ugh, another one of these "oh no poor me I’m on a drug that works" sob stories. You think you’re special? I’ve got a cousin who took this for 15 years while working 80-hour weeks and never missed a day. You’re not sick-you’re weak. Get a spine. Also, probiotics? Really? Next you’ll be rubbing CBD oil on your colon.
Dion Hetemi
November 26, 2025 AT 21:59Let’s be real: if you’re still on azathioprine after 8 weeks with persistent nausea, you’re not managing side effects-you’re ignoring a red flag. And if your doctor hasn’t ordered TPMT/NUDT15 testing by now? They’re either lazy, outdated, or both. This isn’t 2005. We have genetic testing. Use it. Or switch. Don’t martyr yourself for a drug that’s supposed to help you live, not just survive.