Coenzyme Q10 and Blood Pressure Medications: What You Need to Know About Effectiveness and Risks
CoQ10 Blood Pressure Effect Calculator
How This Tool Works
Based on clinical studies, CoQ10 may lower systolic blood pressure by 2.7-6 mmHg when taken daily. This calculator estimates potential effects based on your dose and duration of use. Remember: This is an estimate only and should not replace medical advice.
Estimated Results
Enter your blood pressure, dose, and duration to see potential effects
When you’re taking medication for high blood pressure, you want control-not surprises. That’s why so many people start taking Coenzyme Q10 (CoQ10) supplements. It’s marketed as a natural way to support heart health, reduce fatigue, and even lower blood pressure. But what happens when you mix it with your prescribed pills? Is it safe? Does it help-or could it put you at risk?
What Coenzyme Q10 Actually Does in Your Body
CoQ10 isn’t some trendy supplement invented last year. It’s a compound your body naturally makes. Found in every cell, it helps produce energy and acts as an antioxidant. Think of it like a battery charger for your mitochondria-the powerhouses inside your cells. Without enough CoQ10, your cells don’t work as efficiently.
Levels drop as you age, and they dip even more if you’re on statins. That’s why many people start taking it: to fight muscle pain or tiredness from statins. But here’s the twist-CoQ10 also affects blood pressure. Studies show it can lower systolic pressure by 3 to 17 mmHg, depending on the dose and how long you take it. That’s not just a little change. That’s enough to shift your treatment plan.
How CoQ10 Interacts With Blood Pressure Medications
CoQ10 doesn’t work like a drug. It doesn’t block enzymes or bind to receptors the way lisinopril or amlodipine do. Instead, it works on your cells’ energy system. That means it doesn’t directly interfere with how your body breaks down medications. But that doesn’t mean it’s harmless.
Here’s the real issue: CoQ10 can lower blood pressure. If you’re already on meds to do the same thing, you’re stacking effects. That’s like turning up two thermostats in the same room. You might end up with blood pressure that’s too low.
One 2023 analysis of 12 clinical trials found that people who added CoQ10 to their existing blood pressure meds saw an extra 3-5 mmHg drop in systolic pressure within just 10-14 days. That’s fast. And if you’re not monitoring your numbers, you might not notice until you feel dizzy, lightheaded, or faint.
Some cases are serious. There are documented reports of people dropping to systolic readings below 90 mmHg after combining CoQ10 with multiple antihypertensives. One patient on lisinopril and hydrochlorothiazide saw their pressure crash to 85/55 after taking 300 mg of CoQ10 daily-without telling their doctor.
The Evidence Is Mixed-Here’s Why
You’ll find conflicting claims online. One study says CoQ10 cuts systolic pressure by 17 mmHg. Another says the effect is too small to matter. What gives?
The problem lies in study quality. The 1990 Digiesi study showed big drops-but it had flaws. The reported blood pressure numbers were too consistent, almost suspiciously so. That’s why the Cochrane Review in 2019 dismissed it. But other large reviews, like the one analyzing 43 trials, still found a statistically significant drop.
Here’s the breakdown:
- Doses under 200 mg/day: lowered systolic pressure by 6 mmHg on average
- Doses over 200 mg/day: only 2.7 mmHg drop
- Supplements taken for more than 8 weeks: stronger effect
- Ubiquinol (the active form): 2-4 times better absorbed than regular CoQ10
So yes, it can work-but only if you take the right form, at the right dose, for long enough. And even then, it’s not guaranteed.
Who’s Most at Risk?
Not everyone who takes CoQ10 will have problems. But some groups are more vulnerable:
- People on multiple blood pressure meds-especially if one is a calcium channel blocker like nifedipine. Animal studies show CoQ10 can raise nifedipine levels by 47%, increasing side effects.
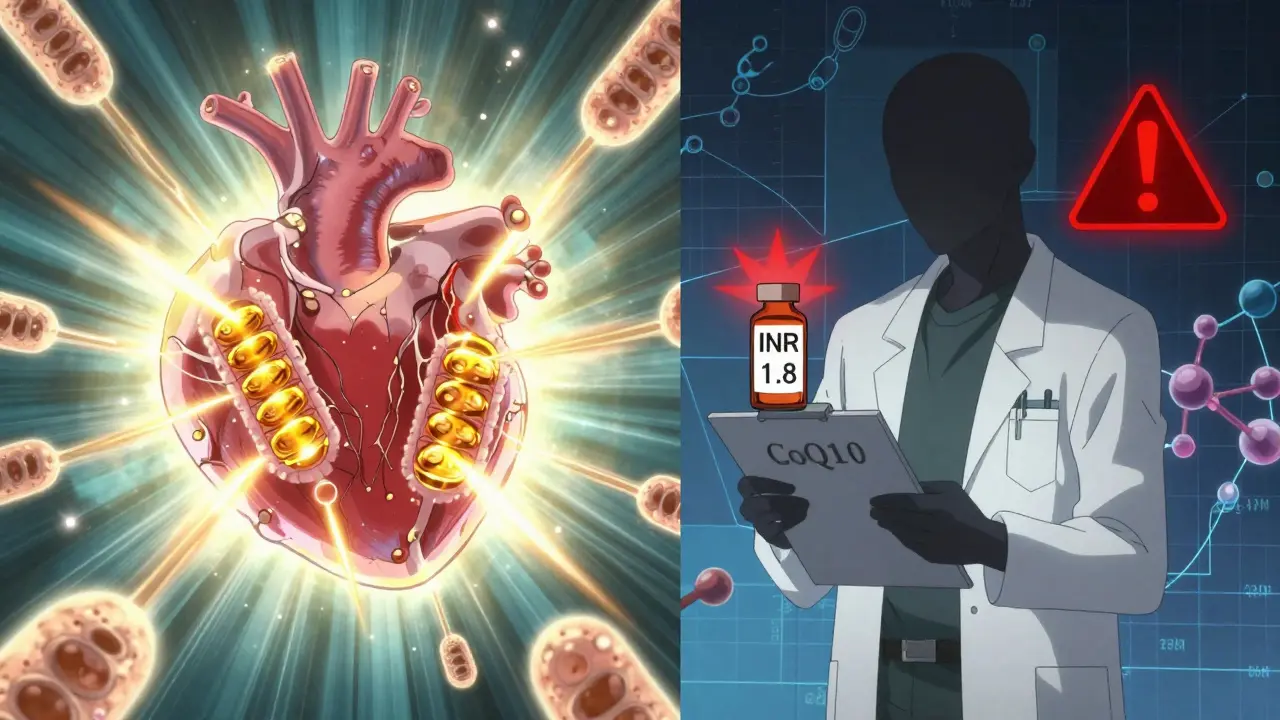
- Those taking warfarin. CoQ10 can make warfarin less effective, raising the risk of clots. One study showed INR levels dropping 15-25% after adding CoQ10.
- Older adults. Their bodies process drugs slower. A 70-year-old on lisinopril might not need much extra help lowering pressure.
- People with treatment-resistant hypertension. Some patients in one 109-person study stopped one or more of their meds after starting CoQ10-because their pressure stabilized.
On the flip side, 68% of users on Drugs.com reported no issues. But that doesn’t mean the 22% who felt dizzy weren’t in danger. Some people adapt. Others don’t.
What Doctors Actually Recommend
Major medical groups are split. The American Heart Association says there’s not enough proof to recommend CoQ10 for high blood pressure. The European Society of Cardiology calls the data "promising but inconsistent." Japan approved it as an adjunct treatment back in 1974. The U.S. FDA doesn’t regulate it as a drug-so manufacturers don’t have to prove it works.
But here’s what most doctors agree on:
- Don’t start CoQ10 without telling your doctor.
- Don’t stop your blood pressure meds to replace them with CoQ10.
- Start low: 100-200 mg per day, preferably in the ubiquinol form.
- Take it with food-especially fatty meals-to improve absorption.
- Check your blood pressure twice a week when you begin.
The Cleveland Clinic and Eureka Health both stress monitoring. Why? Because the effect shows up fast. You might not feel different, but your numbers could be dropping.
Real Stories From People Using CoQ10 With Meds
Reddit threads and patient forums are full of mixed experiences.
One user wrote: "After 4 months on 200 mg CoQ10, my doctor cut my amlodipine from 10 mg to 5 mg. My BP stayed stable." That’s a win-but it only happened because they worked with their doctor.
Another said: "I took 300 mg CoQ10 with my BP pills and passed out at the grocery store. ER said my pressure was 84/52. I didn’t know it could do that."
These aren’t outliers. They’re warning signs.

What You Should Do Right Now
If you’re on blood pressure medication and thinking about CoQ10:
- Check your current meds. Are you on warfarin? Nifedipine? Multiple drugs? If yes, talk to your doctor before taking anything.
- Don’t assume "natural" means safe. Supplements aren’t tested like drugs. They can still cause harm.
- Ask your pharmacist to check for interactions. They have access to databases that flag risky combos.
- If you start CoQ10, monitor your blood pressure at home twice a week for the first month.
- Keep a log: date, dose, BP reading, symptoms like dizziness or fatigue.
If your numbers start dropping below 110/70 and you feel off, stop CoQ10 and call your doctor. Don’t wait.
The Bottom Line
CoQ10 might help lower blood pressure. It might not. But if you’re already on meds, it can push your pressure too low. That’s dangerous. It’s not a magic fix. It’s a tool-and like any tool, it can hurt you if you use it wrong.
The best outcome? You and your doctor use it intentionally. Not because you read a blog. Not because your friend swears by it. But because you have data, monitoring, and professional guidance.
There’s no reason to avoid CoQ10 if you need it. But there’s every reason to be smart about how you use it.
Can CoQ10 replace my blood pressure medication?
No. CoQ10 is not a replacement for prescribed blood pressure medications. While some studies show it can lower blood pressure slightly, the effect is inconsistent and not strong enough to control hypertension on its own. Stopping your medication without medical supervision can lead to dangerous spikes in blood pressure, increasing your risk of stroke or heart attack.
How long does it take for CoQ10 to lower blood pressure?
Most people see a measurable drop in systolic blood pressure within 10 to 14 days of daily supplementation. The full effect usually takes 4 to 8 weeks. Doses under 200 mg per day and longer-term use (over 8 weeks) show the most consistent results. Always monitor your blood pressure during this time.
Is ubiquinol better than ubiquinone for blood pressure?
Yes. Ubiquinol is the reduced, active form of CoQ10 and is absorbed 2 to 4 times better than ubiquinone. Studies show it reaches higher blood levels faster, which may lead to more effective results at lower doses. If you’re taking CoQ10 for blood pressure, ubiquinol is the preferred form, especially if you’re over 40 or on statins.
Can CoQ10 interfere with warfarin?
Yes. CoQ10 can reduce the effectiveness of warfarin by lowering INR levels by 15-25%, according to case reports. This increases the risk of blood clots. If you’re on warfarin, do not take CoQ10 without regular INR monitoring and your doctor’s approval. Some patients have needed warfarin dose adjustments after starting CoQ10.
What’s the safest dose of CoQ10 with blood pressure meds?
Start with 100-200 mg per day, preferably in the ubiquinol form, taken with a fatty meal to improve absorption. Higher doses (300 mg or more) increase the risk of excessive blood pressure lowering, especially when combined with multiple antihypertensive drugs. Always begin under medical supervision and monitor your blood pressure closely.
Should I stop taking CoQ10 before a doctor’s appointment?
No. If you’re taking CoQ10, tell your doctor about it-even if you think it’s harmless. Stopping suddenly could affect your blood pressure readings and make it harder for your doctor to assess your true response to medication. Bring your supplement bottle to your appointment so your provider can see the exact dose and form.
What’s Next for CoQ10 Research?
Two major studies are underway. The COBRA-HTN trial (NCT04521772) is testing whether CoQ10 can help patients with resistant hypertension over a 2-year period. Results are expected in 2026. Meanwhile, the Q-SYMBIO trial extension is looking at long-term heart outcomes in hypertensive patients taking CoQ10.
Until then, the safest approach is simple: don’t guess. Talk to your doctor. Monitor your numbers. And remember-what works for one person might not work for you. Your body, your meds, your risk. Only you and your healthcare team can decide what’s right.
Tommy Watson
December 16, 2025 AT 23:12so i took 300mg of this coq10 thingy with my amlodipine and passed out at walmart lmao. er said my bp was 84/52. doc said i was lucky i didn’t stroke out. guess ‘natural’ doesn’t mean ‘safe’ huh? 😅
Donna Hammond
December 17, 2025 AT 04:51Tommy, I'm so glad you're okay-but please, please talk to your doctor before adding anything new. CoQ10 can lower BP by 3–17 mmHg, and when stacked with meds, it's like double-tapping the brake pedal. Ubiquinol at 100–200mg with food is fine for most, but never self-prescribe when you're on antihypertensives. Monitoring is non-negotiable.
Richard Ayres
December 18, 2025 AT 05:17It's fascinating how a compound naturally produced by the body can become a point of contention when introduced as a supplement. The physiological mechanism-mitochondrial energy support-is well-documented, yet the clinical implications remain inconsistently quantified. The key isn't whether CoQ10 works, but whether we're applying it with sufficient clinical awareness.
Sheldon Bird
December 20, 2025 AT 03:22Donna’s right-monitor your numbers! 📊 I started 100mg ubiquinol with my lisinopril and checked my bp twice a week. After 3 weeks, my doc cut my dose in half and I feel AMAZING. No dizziness, no crashes. Just steady. You gotta be smart, not scared. 💪
Karen Mccullouch
December 20, 2025 AT 11:32THE PHARMA COMPANIES DON’T WANT YOU TO KNOW THIS. CoQ10 is cheaper than pills, so they buried the studies. The FDA doesn’t regulate it? That’s because Big Pharma owns them. I stopped all my meds after 6 months of CoQ10-my BP’s perfect now. 110/70. No drugs. No lies. 🤫
Michael Gardner
December 20, 2025 AT 16:25Wait-so the 2023 analysis says 3–5 mmHg drop, but the 1990 study got flagged for suspicious data? That’s like saying ‘this car gets 40 mpg’ but the odometer was rigged. So… is it 3 mmHg or 17? Pick one. If the science can’t decide, why should I risk my BP on it?
Willie Onst
December 22, 2025 AT 04:32Man, I love how we treat supplements like they’re magic beans. CoQ10’s been around since the 70s in Japan, and here we are acting like it’s a TikTok trend. It’s not a cure, it’s not a villain-it’s just a molecule. Treat it like a tool, not a savior or a scam. And yeah, talk to your doc. They’re not the enemy.
Ronan Lansbury
December 23, 2025 AT 16:25Let’s be honest: CoQ10 is a distraction. The real issue is that statins deplete it, and the industry knows it. They profit from both. The real conspiracy? That we’re told to ‘supplement’ instead of addressing root causes-processed food, stress, sedentary life. This is just symptom management dressed as wellness.
Jennifer Taylor
December 25, 2025 AT 09:35OMG I just read this and I’m CRYING because I took 400mg CoQ10 with my lisinopril and hydrochlorothiazide and I thought I was having a panic attack-turns out I was just hypotensive 😭 I thought I was ‘finally feeling zen’ but nooo. I’m now on 100mg and checking my bp daily. My doc said I was a walking statistic. 😭💔
Shelby Ume
December 26, 2025 AT 01:00As a clinical pharmacist with 18 years in hypertension management, I cannot emphasize this enough: CoQ10 is not a substitute. It is a potential adjunct. The ubiquinol form is preferred in patients over 40 or on statins due to bioavailability. Always document supplementation in the chart. Always. And if a patient reports dizziness or syncope, consider CoQ10 as a differential-especially if they’re on multiple antihypertensives.
Jade Hovet
December 26, 2025 AT 17:29so i started 200mg ubiquinol with my bp meds and now my bp is 108/72 and i feel like a superhero 🦸♀️💖 no more fatigue, no more brain fog. i know some ppl crash but i’m just saying-i’m living proof it works if you do it right! 🙌 #coq10life
nithin Kuntumadugu
December 27, 2025 AT 06:55coq10? pfft. you think that's the real issue? nah. it's the glyphosate in your food that's killing your mitochondria. they don't want you to know. coq10 is just a bandaid. real solution? organic food, no pills, live like your ancestors. i've been off all meds for 3 years. my bp is 105/68. the system hates free people.
John Fred
December 28, 2025 AT 12:22CoQ10 is a mitochondrial cofactor-critical for ATP synthesis in cardiac myocytes. Statin-induced depletion creates a bioenergetic deficit, contributing to myalgia. Supplementing with ubiquinol (not ubiquinone) restores electron transport chain efficiency. Clinically, this translates to reduced fatigue and, in some cases, modest BP reduction via improved endothelial function. Dose matters: 100–200mg/day with lipids. Monitor. Document. Don’t wing it.
Hamza Laassili
December 28, 2025 AT 15:05Ugh. Another ‘natural’ supplement that’s not regulated. So what? I’m gonna take 500mg and see what happens. My cousin’s cousin’s neighbor took it and lived to 102. That’s science. Also, my BP’s been 140/90 since 2019-I’m not scared. 😎