COMISA: How to Manage Insomnia and Sleep Apnea Together

Imagine lying awake at night, your mind racing, while your breathing keeps stopping and starting. You’re not alone. About 45% of people diagnosed with sleep apnea also struggle with chronic insomnia. This isn’t just bad luck-it’s a real, recognized condition called COMISA: Comorbid Insomnia and Sleep Apnea. And treating one without the other? That’s like trying to fix a leaky roof while ignoring the mold growing underneath.
What Is COMISA, Really?
COMISA isn’t just having two sleep problems at once. It’s when insomnia and obstructive sleep apnea (OSA) feed off each other. You might fall asleep fine, but then wake up 10 times an hour because your airway collapses. Or you might sleep through the night but wake up at 3 a.m. and can’t get back to sleep-even with your CPAP on. That’s COMISA.This isn’t rare. Research from Flinders University in Australia shows that between 39% and 58% of people with sleep apnea also have clinical insomnia. That’s nearly half of all OSA patients. Yet, most doctors still treat them as separate problems. One treats the breathing with a CPAP machine. The other prescribes sleep meds for insomnia. Neither fixes the real issue: the two conditions are tangled together.
Why CPAP Alone Fails in COMISA
CPAP is the gold standard for sleep apnea. When used correctly, it works 85-90% of the time. But in COMISA patients, adherence drops to just 42.7%. Why? Because CPAP can make insomnia worse.The mask feels claustrophobic. The air pressure wakes you up. The hose tangles. You start associating your bed with frustration, not sleep. A 2022 survey of over 1,200 COMISA patients found that 68% stopped using CPAP within six months-unless they got help for their insomnia at the same time.
Even when people stick with CPAP, their insomnia often doesn’t improve. The Sleep Heart Health Study showed that 39% of OSA patients still had trouble sleeping after months of CPAP use. That’s because CPAP fixes breathing, but not the mental habits that keep you awake.
Why CBT-I Alone Isn’t Enough
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most effective treatment for insomnia, helping 70-80% of people. It teaches you to break the cycle of worrying about sleep, reduce time in bed when you’re not sleeping, and retrain your brain to associate bed with rest.But if you have sleep apnea, CBT-I alone won’t fix the breathing pauses that keep waking you up. You might learn to sleep better-but if your oxygen levels drop every 45 seconds, your body will still be in survival mode. Your brain won’t let you reach deep, restorative sleep. And without fixing the apnea, you’re still at risk for high blood pressure, heart attacks, and stroke.
The Only Proven Solution: Do Both at Once
The breakthrough came when researchers stopped treating these conditions one after the other-and started treating them together.Dr. Alexander Sweetman’s team at Flinders University ran multiple trials showing that combining CBT-I with CPAP from day one leads to dramatically better results. In one study, 63% of COMISA patients saw their insomnia go into remission after 12 weeks of combined treatment. With CPAP alone? Only 29% improved.
And it’s not just about sleep quality. CPAP usage jumped by an average of 1.2 hours per night when paired with CBT-I. That’s not a small gain-it’s the difference between barely surviving the night and actually feeling rested in the morning.
The secret? CBT-I helps patients tolerate CPAP. It teaches them to stop fighting the machine, to relax into it, and to reframe the discomfort as part of healing-not punishment. One patient on a sleep forum described it this way: “I used to hate my CPAP. After CBT-I, I started looking forward to putting it on. It felt like a tool, not a cage.”
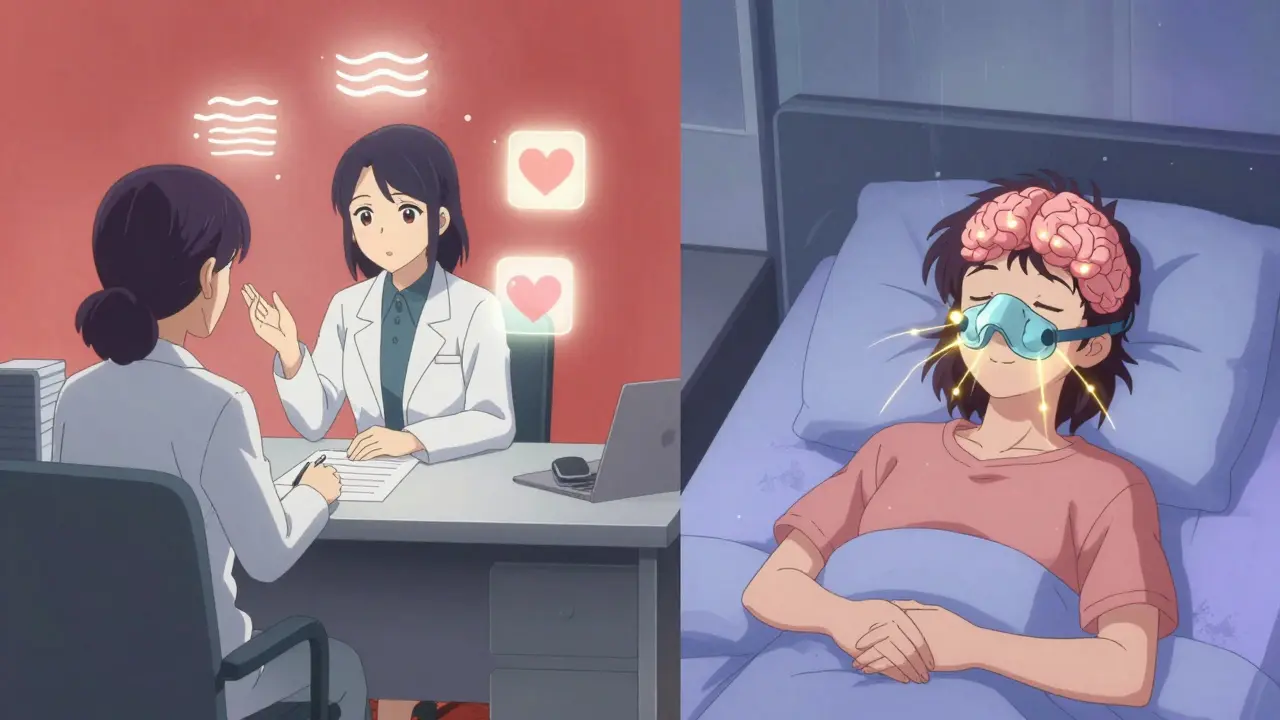
What Does Combined Treatment Look Like?
It’s not complicated, but it does require coordination. Here’s how it works in practice:- Diagnosis: You need a sleep study (polysomnography) to confirm OSA (AHI ≥5) and an Insomnia Severity Index (ISI) score of 15 or higher to confirm clinical insomnia.
- Start CPAP and CBT-I together: No waiting. No “try CPAP first.” You begin both treatments on the same day.
- Modify CBT-I for CPAP users: Standard CBT-I doesn’t account for mask discomfort or pressure-related awakenings. Specialized protocols address these directly-like using stimulus control to rebuild positive associations with bed, even with the machine on.
- Use a sleep coach: Trained professionals guide you through both treatments. They help you adjust pressure settings, troubleshoot mask leaks, and reframe anxious thoughts about sleep.
A 2020 trial showed that patients who got five sessions of combined CBT-I and CPAP coaching improved their insomnia by 54% and added over an hour of CPAP use per night-six months later.
What About Digital CBT-I?
Apps like Sleepio and Somryst now offer digital CBT-I programs. Some even integrate with CPAP data to personalize advice. These are great for mild cases or people in rural areas with no sleep specialists nearby.But they’re not for everyone. A 2023 study in JAMA Network Open found that digital CBT-I worked well for COMISA patients with mild OSA (AHI 5-15)-65% saw remission. But for moderate to severe OSA (AHI >15), success dropped to 38%. Why? Because the physical disruption from apnea is too strong to fix with an app alone.
That’s why the best results still come from working with a trained psychologist who understands both insomnia and sleep apnea. If you’re struggling with severe breathing issues, don’t rely on an app. Get human support.
Other Treatments? Orexin Antagonists, Mandibular Devices, Neurostimulation
There are other options-but they’re not first-line.Orexin antagonists like suvorexant (recently FDA-approved for COMISA in December 2023) help you stay asleep by blocking brain signals that keep you awake. In trials, they improved sleep maintenance in 57% of COMISA patients when used with CPAP. But they’re expensive, can cause next-day drowsiness, and aren’t recommended for long-term use.
Mandibular advancement devices (mouthpieces) work for mild to moderate OSA, but they don’t help with insomnia. They’re not a substitute for CPAP in moderate-severe cases.
Neurostimulation (like hypoglossal nerve stimulation) is an implantable device for severe OSA patients who can’t tolerate CPAP. But it doesn’t address insomnia at all. And it’s invasive, expensive, and only for a small subset.
Right now, the only treatment with strong, repeated evidence for COMISA is CBT-I + CPAP. Everything else is a backup plan.

Why Don’t More Doctors Treat COMISA This Way?
Because most don’t know how.A 2022 survey of U.S. sleep centers found that only 28% had formal referral pathways between sleep physicians and behavioral sleep specialists. Most patients get referred to one specialist, then the other-months apart. The average wait time to see a CBT-I-trained psychologist? 14.3 weeks.
Even when doctors know about COMISA, they often don’t have the resources. CBT-I requires 40-60 hours of specialized training. Few psychologists have it. Few sleep labs coordinate with them.
But things are changing. In January 2024, Medicare introduced new billing codes (G2212-G2214) specifically for integrated COMISA treatment. That means clinics can now get paid for doing it right.
Insurance companies are noticing the savings too. UnitedHealthcare found that COMISA patients on combined treatment used 22% less healthcare overall-saving $1,843 per person per year. That’s not just better sleep. That’s fewer ER visits, fewer heart problems, fewer missed workdays.
What If You’re Already on CPAP and Still Can’t Sleep?
If you’ve been using CPAP for months and still wake up at 3 a.m. every night, you might have COMISA. Here’s what to do next:- Take the Insomnia Severity Index (ISI) test online-it’s free and takes 2 minutes.
- If your score is 15 or higher, ask your sleep doctor for a referral to a psychologist trained in CBT-I.
- Don’t wait. The longer you go without treating both, the harder it gets to break the cycle.
- Track your CPAP usage. If you’re using it less than 4 hours a night, you’re not getting the benefit-and your insomnia is likely making it worse.
One patient, a 58-year-old teacher from Hobart, told me: “I was on CPAP for two years. I still felt exhausted. I thought I was broken. Then I got CBT-I. Now I sleep 7 hours. I don’t even notice the machine anymore.”
The Bigger Picture: COMISA Is the Future of Sleep Medicine
Sleep medicine is moving away from siloed care. COMISA is a model for how we treat other overlapping conditions-like depression and chronic pain, or anxiety and IBS.By 2027, nearly 40% of U.S. sleep centers plan to offer integrated COMISA programs. The American Academy of Sleep Medicine now officially recommends it. And with new AI tools predicting who will respond best to combined therapy, we’re getting closer to truly personalized sleep care.
But right now, the biggest barrier isn’t science. It’s access. Only 1% of people with insomnia ever get CBT-I. And only 18% of COMISA patients get treated with both therapies.
If you’re one of them, you don’t need to wait. Ask for help. Demand coordination. Push for both treatments together. Because sleep isn’t just about breathing-or just about falling asleep. It’s about both. And you deserve to get both right.
What is COMISA?
COMISA stands for Comorbid Insomnia and Sleep Apnea. It’s when a person has both chronic insomnia and obstructive sleep apnea at the same time. It’s not just having two sleep problems-it’s when they interact and make each other worse. About 40-58% of people with sleep apnea also have clinical insomnia, making COMISA one of the most common but under-treated sleep disorders.
Can CPAP cure insomnia?
No. CPAP fixes breathing pauses during sleep, which helps with sleep apnea, but it doesn’t address the psychological and behavioral patterns that cause insomnia. In fact, many people with COMISA find CPAP makes their insomnia worse due to mask discomfort, noise, or anxiety around the device. Treating insomnia requires CBT-I-cognitive behavioral therapy specifically designed for sleep problems.
Can CBT-I cure sleep apnea?
No. CBT-I helps you fall asleep faster and stay asleep longer by changing thoughts and habits around sleep, but it doesn’t stop your airway from collapsing at night. That’s what CPAP or other medical devices are for. However, CBT-I can reduce OSA severity by up to 15% by consolidating sleep and reducing nighttime awakenings, which lowers the number of apneas.
Is it better to treat sleep apnea first or insomnia first?
Research shows that treating them together works best. Treating sleep apnea first with CPAP often fails because insomnia makes people reject the machine. Treating insomnia first leaves the breathing problems untreated, which still harms your heart and brain. The strongest evidence supports starting both CBT-I and CPAP at the same time-this leads to the highest success rates in both sleep quality and device adherence.
How long does COMISA treatment take?
Most people see improvements in 6-12 weeks. CBT-I typically involves 5-8 sessions over 6-8 weeks. CPAP adaptation happens within the first 2-4 weeks, especially with coaching. After 12 weeks, most patients report significantly better sleep, higher CPAP use, and reduced daytime fatigue. Long-term success depends on sticking with both treatments.
Are there any new treatments for COMISA in 2025?
Yes. In December 2023, the FDA approved suvorexant, an orexin antagonist, specifically for COMISA patients using CPAP. New CPAP machines like ResMed’s AirSense 11 adjust pressure automatically based on sleep stage. Digital CBT-I platforms now sync with CPAP data to give real-time feedback. Research is also underway using AI to predict which patients will respond best to combined treatment-making care more personalized than ever.
How do I find a doctor who treats COMISA?
Ask your sleep specialist if they work with a behavioral sleep medicine psychologist. Look for clinics that mention “integrated sleep care” or “comorbid insomnia and sleep apnea” on their website. You can also check the American Academy of Sleep Medicine’s directory for CBT-I-certified providers. If you’re in a rural area, ask about telehealth options for CBT-I-many programs now offer remote sessions with CPAP data integration.
What’s Next? Don’t Wait for the System to Catch Up
You don’t need to wait for your doctor to know about COMISA. You don’t need to wait for insurance to cover everything. You just need to ask for both treatments-CBT-I and CPAP-together.Keep a sleep diary. Track your CPAP usage. Score your insomnia with the ISI. Bring it to your next appointment. Say: “I think I have COMISA. I want to try CBT-I and CPAP at the same time.”
This isn’t just about sleep. It’s about your heart, your mood, your energy, your life. And you deserve to feel rested-not just surviving the night, but truly waking up.
Michael Dillon
December 26, 2025 AT 02:56Let me be the first to say this: CPAP is a glorified torture device. I’ve worn one for three years. I still wake up with a headache, a dry throat, and the lingering feeling that my face is being held hostage by plastic. And now you want me to add therapy on top? No thanks. I’d rather just nap in my car during lunch.
Gary Hartung
December 27, 2025 AT 06:25Oh, absolutely. The ‘integrated’ approach. How quaint. As if sleep medicine were some kind of symphony where CBT-I and CPAP dance in perfect harmony-when in reality, it’s two broken instruments being forced into the same room by a bureaucrat with a clipboard and a grant proposal. The fact that we’re even debating this in 2024 is a testament to how little progress we’ve made. Truly, the golden age of sleep science.
Ben Harris
December 28, 2025 AT 12:22People don't get it. You can't fix insomnia with talk therapy if your airway keeps collapsing. That's like trying to fix a broken leg with affirmations. CPAP is the only thing that stops you from dying in your sleep. The rest is just noise. And don't get me started on those apps. I downloaded one. It told me to breathe deep. I died. Just kidding. But seriously. This is why medicine sucks.
Oluwatosin Ayodele
December 29, 2025 AT 11:30Here in Nigeria we don't have CPAP machines in most clinics. We have prayer and herbal tea. But I’ve read your studies. You’re right. COMISA is real. But your solution assumes wealth. Access. Infrastructure. I have a cousin who wakes up choking every night. He sleeps sitting up. He doesn’t have a therapist. He has a cell phone and a YouTube video titled 'How to Stop Snoring in 7 Days.' You think CBT-I helps him? No. He needs a machine. Not a mindset.
Jason Jasper
December 29, 2025 AT 11:44I’ve been on CPAP for four years. I tried CBT-I last year. It didn’t magically fix me. But it made me stop hating the machine. That’s huge. I used to see it as an enemy. Now I see it as a roommate who’s weird but reliable. The therapist helped me reframe the noise, the mask, the feeling of being trapped. It’s not a cure. But it’s a peace treaty. And sometimes that’s enough.
Mussin Machhour
December 29, 2025 AT 22:03Yo. I was skeptical too. But I did the combo. 5 sessions of CBT-I + CPAP from day one. First week? Still hated the mask. Week 3? Started falling asleep faster. Week 6? I actually looked forward to bedtime. Now I sleep 7 hours. No meds. No drama. Just a machine and a therapist who didn’t judge me for crying because I couldn’t sleep. If you’re still awake at 3 a.m. and your CPAP’s collecting dust-just try it. You’ve got nothing to lose except insomnia.
Winni Victor
December 30, 2025 AT 21:36Oh sweet merciful god, another ‘integrated treatment’ article. Like we didn’t already know that combining things works better than doing them separately. Did we need a 2000-word manifesto to tell us that? I mean, if you combine peanut butter and jelly, you get a sandwich. Who knew? Also, why is everyone so obsessed with CPAP? I just wear a nasal strip and pray. Works fine.
Terry Free
January 1, 2026 AT 19:14CBT-I? Please. That’s just cognitive behavioral nonsense wrapped in clinical jargon. You’re telling me I need to ‘reframe my relationship with the mask’? I need to stop my airway from collapsing. That’s not a thought problem. That’s a physics problem. And if you think a therapist can fix that, you’ve been reading too many wellness blogs. CPAP is medicine. CBT-I is a spa day for your brain.
Lindsay Hensel
January 2, 2026 AT 00:38Thank you for this comprehensive, evidence-based exposition. It is both scientifically rigorous and profoundly human. The integration of behavioral and physiological interventions represents not merely an advancement in clinical practice, but a moral imperative. Sleep is not a luxury. It is the foundation of human dignity. We owe it to our patients to offer them both.
Sophie Stallkind
January 3, 2026 AT 04:50My husband has COMISA. We tried CPAP alone for 18 months. He stopped using it. Then we found a specialist who did both. He’s now using CPAP 6.5 hours a night. He sleeps through the night. He doesn’t yell at me at 3 a.m. anymore. I cried when he told me he felt rested. This isn’t just medical. It’s relational. It’s life-changing.