Crossing Time Zones with Insulin: Adjusting Doses Safely for Travel

Time Zone Insulin Adjustment Calculator
Note: Always consult your healthcare provider before adjusting insulin. This tool provides general guidance based on CDC recommendations.
When you’re flying across time zones with diabetes, your body doesn’t care about your flight schedule. Your insulin does. Skip the adjustment, and you could wake up in Tokyo with a blood sugar of 30 mg/dL-or land in New York with one at 400 mg/dL. Neither is safe. And neither is rare. Around 7 million insulin users cross three or more time zones every year. Most don’t plan ahead. That’s where things go wrong.
Why Time Zones Break Your Insulin Routine
Your insulin schedule is built around a 24-hour day. Basal insulin works steadily. Bolus insulin matches meals. When you fly east, the day gets shorter. You skip hours of daylight, but your body still needs fuel. If you keep dosing like normal, you risk hypoglycemia. Fly west? The day stretches out. You’ve got extra hours between meals. Without extra insulin, your blood sugar climbs. This isn’t theoretical. A 2019 study of 450 travelers found 12% had rebound high blood sugar from unnoticed nighttime lows-called the Somogyi effect-after skipping dose adjustments.Eastbound Travel: Shorter Days, Less Insulin
Going from London to Tokyo? You lose 9 hours. Your body thinks it’s 3 a.m. when it’s actually noon. Your usual bedtime basal dose? It’s now hitting you in the middle of your active day. That’s too much. The fix? Reduce your long-acting insulin by 20-33% on the travel day. For example, if you normally take 20 units of glargine at night, drop to 14-16 units. Keep your mealtime insulin the same-just shift the timing to match local meals. Don’t skip meals just because it’s "early" in your old time zone. Eat when the sun’s up where you are.Westbound Travel: Longer Days, More Insulin
Flying from New York to Honolulu? You gain 5 hours. Now you’ve got an extra meal window. Your usual three meals turn into four. Your body needs more insulin. The standard advice: add one extra rapid-acting insulin dose 4-6 hours after your third meal. That dose should be about half your usual meal bolus. So if you normally take 8 units for dinner, take 4 extra units later. Don’t just wait and hope your blood sugar stays normal. You’ll end up with a spike you didn’t see coming.Pump Users: Don’t Just Flip the Clock
If you use an insulin pump, changing the time setting all at once isn’t always safe. For time changes under 2 hours, just update the pump when you land. For bigger jumps-say, 6+ hours-do it in stages. Change the pump time by 2 hours each day until you’re synced. Why? A 2021 UCLA study showed this method cut hypoglycemic events by 27% compared to jumping straight to destination time. But if you’re used to tight control and your pump has automated features like Control-IQ, switching immediately might work better. The tech adjusts basal rates automatically based on glucose trends. Still, test your blood sugar every 2-3 hours for the first 24 hours, no matter what.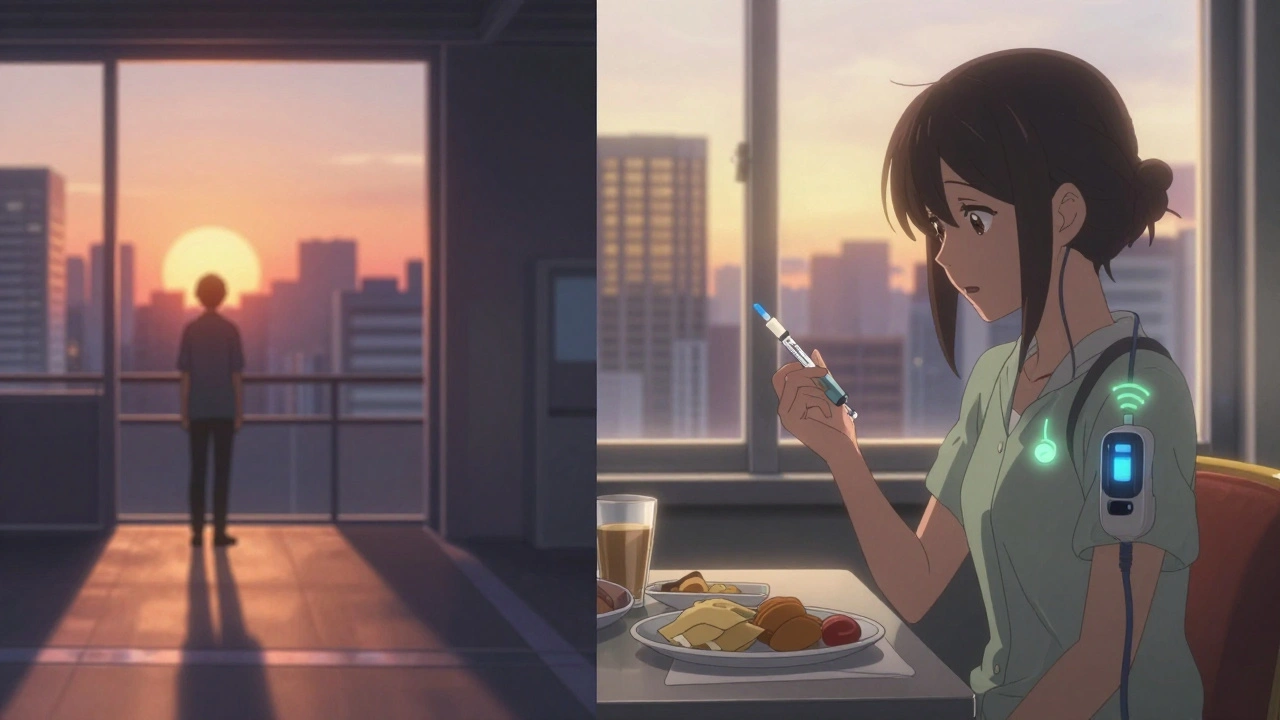
What the Experts Really Say
Dr. David Edelman from Duke University says it best: "Routine matters more than perfect timing." Don’t stress about matching your home schedule exactly. Focus on eating meals at consistent times in the new time zone. Keep snacks handy. Carry glucose tabs. And for the first 24-48 hours, aim for a slightly higher target: 140-180 mg/dL. Dr. Howard Wolpert’s research showed this buffer cuts severe lows by 41%. It’s not about being perfect. It’s about staying safe.Flight Risks: Dehydration and Absorption
Cabin pressure and dry air during long flights change how your body handles insulin. A 2025 Aerospace Medical Association report found insulin absorption can increase by 15-20% mid-flight. That means your usual bolus might hit harder than expected. To compensate, reduce your mealtime insulin by 10-15% during flights longer than 6 hours. Also, drink water. Dehydration thickens your blood, which can raise glucose levels and make insulin less effective. Avoid alcohol and caffeine-they worsen dehydration.Insulin Storage: Heat Kills Potency
Insulin doesn’t like heat. If your bag sits in a hot airport or gets left in a car, it loses potency. At 86°F (30°C), insulin degrades 15% per day. Carry it in a cooling pouch or insulated bag. Never check it in luggage. TSA lets you bring insulin, syringes, and pumps through security without limits-but you need a doctor’s letter. Travelers with letters report 89% fewer delays. Print one. Keep it in your wallet.How Much Extra Insulin Should You Bring?
Always pack 20-30% more than you think you’ll need. Delays happen. Time zones confuse your schedule. You might need an extra dose. One user on Reddit lost her insulin bag during a layover and ended up in the ER with diabetic ketoacidosis. Don’t be that person. Bring extra pens, vials, syringes, and test strips. Store them separately-don’t keep all your supplies in one bag. Keep half in your carry-on, half in your checked luggage. And if you’re flying internationally, know the local name for insulin. In Germany, it’s "Insulin"-same as English. In Japan, it’s "インスリン". Save the translation.
What Works Best? Real User Data
A review of 327 traveler reports on Diabetes Hands Foundation found 68% had better results when they switched to destination time immediately upon departure-not arrival. They set their watches, pumps, and alarms to local time as soon as they boarded. They ate meals at local times, even if it meant breakfast at 11 p.m. Their blood sugars stayed steadier. The other 32% tried gradual changes and ended up dosing twice in one day or missing doses entirely. Don’t overcomplicate it. Change your clock. Eat when it’s local time. Dose accordingly.Technology Is Making This Easier
New tools are cutting the guesswork. The t:slim X2 pump with Control-IQ detects time zone changes via GPS and adjusts basal rates automatically. Clinical trials showed a 63% drop in manual dosing errors. The European Association for the Study of Diabetes now recommends CGM for all insulin users crossing three or more time zones. Real-time glucose data cuts severe lows by 58%. And by 2025, smart pens from Ypsomed will calculate dose adjustments based on your flight path and direction. You won’t have to do the math yourself.Plan Ahead-4 Weeks Before You Go
This isn’t something you wing. Talk to your diabetes care team at least four weeks before departure. They’ll help you build a plan based on your insulin type, daily pattern, and travel route. Patients who do this have 53% fewer diabetes-related disruptions during travel. That means fewer ER visits, fewer canceled plans, and less stress.Final Checklist Before You Fly
- Get a doctor’s letter for TSA (print two copies)
- Bring 20-30% extra insulin and supplies
- Use a cooling pack for insulin in hot climates
- Set your watch, pump, and phone to destination time at takeoff
- Adjust basal insulin down for eastbound, up for westbound
- Carry fast-acting glucose (tabs, juice, gel)
- Wear a medical ID bracelet
- Know the emergency number in your destination country
Traveling with insulin isn’t about perfection. It’s about preparation. You don’t need to be a scientist. You just need to know your numbers, respect the clock, and plan like your health depends on it-because it does.
Rashmi Gupta
December 7, 2025 AT 06:02So let me get this straight-you’re telling me I should just flip my pump clock mid-flight and eat dinner at 11 p.m. because the sun’s up in Tokyo? That’s not preparation, that’s surrender. My body doesn’t care about your GPS-tracked time zones. It cares about rhythm. And rhythm isn’t a setting you change with a firmware update.
Annie Gardiner
December 8, 2025 AT 01:44Wait, so if I’m flying west and I add a half-bolus, does that mean I’m basically insulin-pumping my way through jet lag? I mean, I get the science, but isn’t this just turning diabetes into a full-time job? I used to just eat, sleep, and fly. Now I’ve got math equations and cooling pouches. I miss when my biggest travel worry was airport food.
Kumar Shubhranshu
December 8, 2025 AT 02:48Mayur Panchamia
December 10, 2025 AT 00:58Kenny Pakade
December 11, 2025 AT 11:22Gwyneth Agnes
December 12, 2025 AT 22:38Ashish Vazirani
December 14, 2025 AT 21:19Let me tell you about the time I flew from Mumbai to Chicago and my insulin went rogue-my pump glitched, my cooling pouch melted in the baggage hold, and the flight attendant thought my glucose tabs were drugs. I had to beg the captain to let me use the galley to test. I cried. I screamed. I ate a whole bag of Skittles just to stay alive. And you? You’re talking about 15% absorption rates like it’s a TED Talk. I survived. But not because of your checklist. Because I refused to die quietly.
Kay Jolie
December 16, 2025 AT 00:33While the piece offers a clinically robust framework for temporal insulin recalibration, it conspicuously neglects the epistemological dissonance inherent in circadian entrainment under artificial temporal displacement. The somatotopic feedback loop between exogenous insulin kinetics and chrono-biological entrainment is not merely a pharmacokinetic variable-it’s a phenomenological rupture in the lived experience of metabolic autonomy. One must ask: are we optimizing for glycemic stability, or merely simulating temporal conformity?
Max Manoles
December 17, 2025 AT 00:26I appreciate the thoroughness of this guide. I’ve been using a t:slim X2 with Control-IQ for two years now, and the automatic adjustments during transcontinental flights have been a game-changer. I do agree with the recommendation to test every 2-3 hours initially-my first trip, I skipped that and ended up with a 300 mg/dL spike at 3 a.m. because I assumed the pump knew better. It didn’t. Human oversight still matters. Also, carrying two separate insulin stashes saved me when my carry-on got delayed in Dubai. I’d add: keep a backup battery for your pump and write down your basal rates in case your screen dies. Simple, but critical.
Arjun Deva
December 18, 2025 AT 12:01Who funded this? Big Pharma? The CDC? The WHO? They want you to buy more pumps, more cooling packs, more test strips. Real diabetics in India don’t have access to any of this. They use refrigerated milk cartons as coolers. They reuse syringes. They fly with one vial and pray. This article is a luxury. And the GPS auto-adjust feature? That’s a surveillance tool. Your pump is tracking your flight path. Who’s watching? Who’s storing your data? You’re not managing diabetes-you’re feeding the algorithm.
Priya Ranjan
December 20, 2025 AT 05:09Of course you need a doctor’s letter. Anyone who doesn’t have one is irresponsible. And bringing extra insulin? That’s not optional-it’s basic hygiene. I’ve seen people show up at clinics after a trip with DKA because they thought ‘it’ll be fine.’ It’s not fine. It’s not even close. You wouldn’t fly without a seatbelt. Why fly without backup insulin? You’re not being careful-you’re being selfish. Your life isn’t yours alone. You have a responsibility to not become a burden. And if you can’t handle that? Don’t travel. Stay home. It’s that simple.
Katie O'Connell
December 21, 2025 AT 21:16While the article presents a comprehensive and empirically grounded framework for temporal insulin modulation during transcontinental travel, it is regretfully devoid of any discussion regarding the socio-economic disparities in access to CGM technology and insulin storage infrastructure. The implicit assumption that all individuals possess the financial means to procure cooling pouches, dual insulin stashes, and smart pumps fundamentally undermines the universality of the guidance. A more equitable framework would incorporate low-resource adaptation protocols-such as the use of evaporative cooling via damp cloth wrapping, or the strategic timing of bolus doses relative to ambient temperature fluctuations-thereby ensuring that safety is not a privilege but a right. Furthermore, the recommendation to ‘set your watch at takeoff’ assumes a uniform cognitive and temporal literacy that may not be universally accessible. A more inclusive approach would involve pre-travel education modules delivered via audio or visual media in local languages, particularly for travelers in low-income nations where digital literacy remains unevenly distributed.