Health Literacy Strategies: How to Read Medication Labels and Avoid Dosing Errors

Medication Dosing Translator
Understand Your Medication Instructions
Medication labels often use confusing medical terms. This tool translates common dosing instructions into plain English so you can take your medicine safely.
Example schedule:
Every year, over 1.3 million people in the U.S. are harmed because they took medicine the wrong way. Not because they were careless - but because they didn’t understand what the label said. You might think reading "take one tablet twice daily" is simple. But for millions of people, it’s not. The average adult reads at a 6th to 8th grade level. Yet most medicine labels are written like a college textbook. That mismatch is deadly.
Why Medication Labels Are So Confusing
Look at a typical prescription bottle. It says: "Take 1 tab PO BID." What does that even mean? "PO"? "BID"? If you’ve never been to medical school, you’re already lost. Even when labels use plain words, they’re still packed with ambiguity. "Take every 4 to 6 hours" - does that mean you can take it at 8 a.m., 12 p.m., and 6 p.m.? Or do you have to wait exactly 4 hours, even if that means waking up at 3 a.m.? "Take with food" - does that mean before, during, or after? A 2009 study found that 47% of patients misunderstood standard instructions like these.It’s worse with liquid medicines. Parents giving cough syrup to kids often mix up "mL" and "mg." One parent told researchers they thought "give 5 mL twice daily" meant 5 mL total - not 5 mL each time. That’s a 100% overdose. And it’s not rare. In one study, 63% of children’s medicine labels used confusing charts instead of simple numbers. Only 8% used pictures. That’s not an accident - it’s a system failure.
What Works: The Science of Clear Labels
There’s good news. We know exactly how to fix this. And it’s not about making labels fancier. It’s about making them simpler.The Universal Medication Schedule (UMS) changed everything. Instead of "twice daily," labels now say: "Take in the morning, at noon, in the evening, at bedtime." No math. No guessing. A 2022 study in Wisconsin found that when pharmacies switched to UMS, dosing confusion dropped by 47% among older adults taking five or more pills a day. One 72-year-old patient said, "I finally understood when to take my pills. Before, I was scared I’d mess up. Now, I just follow the time of day."
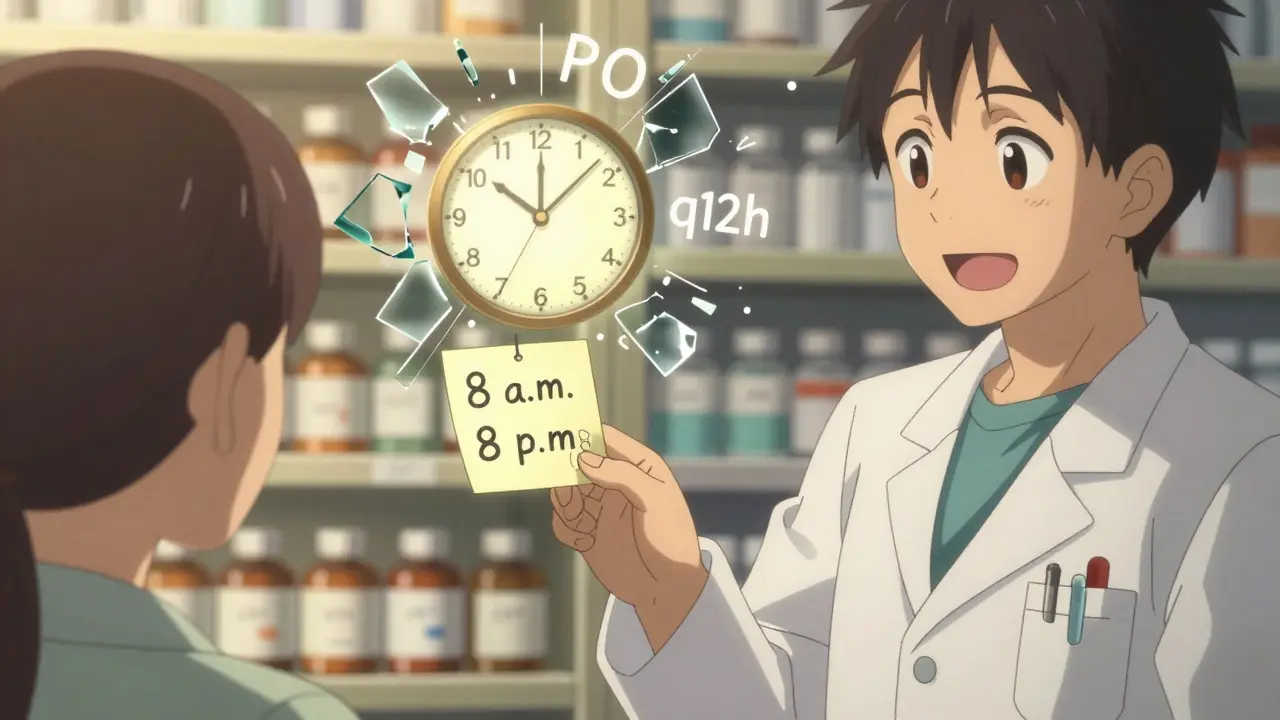
Another proven fix? Pictograms. Simple drawings of a person taking a pill, a clock, or a food plate. A 2023 study showed these increased correct understanding by 28% for people with low literacy. The U.S. Pharmacopeia now requires them on all prescription labels by May 2025. Why? Because a picture of a clock with "8 a.m." is clearer than "q12h."
And then there’s the language itself. The Institute for Safe Medication Practices says everything should be written at a fifth-grade reading level. That means short sentences. Active voice. No jargon. "Take one pill" instead of "Administer one tablet orally." "Do not drink alcohol" instead of "Avoid concomitant ingestion of alcoholic beverages." Merck’s team tested this - their simplified labels hit 92% comprehension across all literacy levels. Their secret? Average sentence length: 8.2 words. 95% of instructions in active voice.
How Patients Get It Wrong - And Why
People don’t make mistakes because they’re dumb. They make them because the system is designed to confuse.One common error: thinking "take twice daily" means "take two pills at once." That’s what 40% of Reddit users in r/Pharmacy say they see weekly. But "twice daily" means two separate doses - not one double dose. Another: confusing "every 4 hours" with "four times a day." The first means you might need to wake up at 2 a.m. The second means 8 a.m., 12 p.m., 4 p.m., 8 p.m. - no middle-of-the-night alarms.
And then there’s the "syringe" problem. A woman in a CDC focus group drank albuterol from the plastic bottle because she thought it was a "syringe." The label didn’t say "oral solution." It didn’t show a picture. She assumed. That’s not negligence. That’s a failure of design.
Even simple terms like "as needed" cause chaos. Does that mean when you feel pain? When it’s bad? When you remember? One patient told researchers she took her pain pill "as needed" 12 times in one day because she didn’t know there was a maximum. That’s how overdoses happen.

What Clinicians Can Do - Even Without New Labels
You don’t need a new pharmacy system to help someone understand their medicine. You just need to talk differently.The teach-back method is the most powerful tool in any clinic. It’s simple: after explaining how to take a pill, ask the patient to show you or tell you how they’ll do it. Not "Do you understand?" - that’s a yes/no trap. Ask: "Can you show me how you’ll take this pill tomorrow?"
A 2023 trial at Children’s Hospital of Philadelphia found that using teach-back with caregivers reduced liquid medication errors by 34%. It only takes 1 to 2 extra minutes per medication. And it works because it catches misunderstandings before the patient leaves.
Another quick win: write the instructions on a sticky note. Not just the dose - the time. "Take 1 tablet at 8 a.m. and 8 p.m." Hand it to them. Say: "This is your plan. Keep it on your fridge."
And don’t forget language. If someone speaks Spanish, give them the label in Spanish. If they’re blind, offer a braille label. If they’re elderly and forgetful, suggest a pill organizer with alarms. One-size-fits-all doesn’t work.
What’s Changing - And What’s Coming
The rules are finally catching up to the science. In May 2023, the U.S. Pharmacopeia made new labeling rules official. By May 2025, every prescription bottle in the U.S. must use UMS times, pictograms, and fifth-grade language. The FDA is pushing drugmakers to test labels with real patients before they go to market.Some hospitals are already ahead. UW Health cut medication-related readmissions by 22% after training staff in health literacy. Malpractice claims dropped 15%. That’s not just better care - it’s cheaper care. Every $1 spent on clear labels saves $3.75 in avoided hospital visits.
What’s next? AI tools that scan labels and explain them in plain language. A new CDC test to measure if patients truly understand their meds. And by 2024, the FDA will require standard pictograms on all prescription containers - no more guessing what the little drawing means.
What You Can Do Today
You don’t have to wait for the system to fix itself. Here’s what you can do right now:- Always ask: "Can you write down when I’m supposed to take this?"
- Use the UMS clock: If the label says "twice daily," assume it means morning and bedtime. Ask to confirm.
- Check the units: Is it "mg" or "mL"? If you’re not sure, call the pharmacy. One wrong digit can kill.
- Use a pill organizer: Even a simple one with AM/PM slots helps. Don’t trust your memory.
- Bring someone with you: When you get a new prescription, take a family member. Two ears are better than one.
- Take pictures: Snap a photo of the label. If you forget, you can look back.
And if you’re a caregiver for a child or older adult: don’t guess. Always double-check the dose. Write it down. Show it to the pharmacist. Ask: "Is this safe?"
It’s Not About Intelligence - It’s About Design
Health literacy isn’t about how smart you are. It’s about whether the system was built for you. You shouldn’t need a degree to know how to take your medicine. You shouldn’t need to be fluent in Latin to understand a pill bottle. The fact that we’ve let this go on for decades is a failure - not of patients, but of design.But change is here. Clear labels. Simple words. Pictures. Teach-back. These aren’t fancy ideas. They’re basic human rights. And they’re working. Every time someone takes their medicine the right way because the label finally made sense - that’s a life saved.
What does "take twice daily" really mean?
"Take twice daily" means two separate doses - one in the morning and one in the evening. It does NOT mean taking two pills at once. For example, if your pill says "take twice daily," you should take one at 8 a.m. and one at 8 p.m. - not two pills at 8 a.m. and none at night. Many people confuse this, leading to overdoses or missed doses. The Universal Medication Schedule (UMS) helps by saying "take in the morning" and "take at bedtime" instead.
How do I know if I’m giving the right dose of liquid medicine?
Always check the unit: "mL" (milliliters) is volume, "mg" (milligrams) is weight. Never use kitchen spoons - they vary too much. Use the measuring cup or syringe that came with the medicine. If it says "give 5 mL twice daily," that means 5 mL each time - not 5 mL total. A 2012 study found 63% of children’s medicine labels confused parents because they used charts instead of clear numbers. If you’re unsure, call the pharmacy. They’ll show you how to measure it correctly.
What should I do if the label uses medical terms like "BID" or "PO"?
Don’t guess. Call the pharmacy and ask for plain English. "BID" means twice daily. "PO" means by mouth. But you shouldn’t have to memorize Latin to take your medicine. Ask them to rewrite the label in simple terms. Most pharmacies will do it - especially if you explain you’re having trouble understanding. Some even offer printed instructions in large print or with pictures.
Can I trust the dosage instructions on over-the-counter medicine?
Not always. A 2012 review found that 18.5% of top-selling children’s cough syrups didn’t list active ingredients on the front. Many used confusing charts instead of clear dosing by age or weight. Always check the "Active Ingredients" section. Look for the amount per mL or per teaspoon. If it’s not clear, don’t guess. Ask a pharmacist. And never give adult medicine to a child - even if you cut the dose in half.
What’s the best way to remember when to take multiple pills?
Use a pill organizer with morning, noon, evening, and bedtime compartments. Set phone alarms labeled with the medicine name and time. Write down your schedule on a sticky note and put it on your mirror or fridge. Ask your pharmacist if your pills can be combined into one daily dose - sometimes they can. The goal is to make it automatic. Don’t rely on memory. Even one missed or doubled dose can cause side effects or reduce effectiveness.
Jane Lucas
December 27, 2025 AT 11:32Anna Weitz
December 28, 2025 AT 17:26Gerald Tardif
December 29, 2025 AT 17:03Elizabeth Ganak
December 30, 2025 AT 15:13John Barron
December 31, 2025 AT 17:30Elizabeth Alvarez
January 2, 2026 AT 01:03Todd Scott
January 2, 2026 AT 02:59Andrew Gurung
January 3, 2026 AT 20:25Paula Alencar
January 4, 2026 AT 11:26Nikki Thames
January 4, 2026 AT 20:47Chris Garcia
January 5, 2026 AT 16:26James Bowers
January 7, 2026 AT 04:57Janice Holmes
January 7, 2026 AT 19:35Olivia Goolsby
January 8, 2026 AT 14:33Alex Lopez
January 9, 2026 AT 20:49