Herpes Simplex Virus: Types, Symptoms, and Antiviral Therapy Explained
Herpes Simplex Virus isn’t just a cold sore or a rash you get once and forget. It’s a lifelong infection that affects nearly 7 out of 10 people under 50 worldwide. And while many think it’s only about mouth sores or sexual transmission, the reality is far more complex - and treatable.
Two Viruses, One Family: HSV-1 and HSV-2
There are two types of herpes simplex virus: HSV-1 and HSV-2. They look almost identical under a microscope - both are enveloped, double-stranded DNA viruses about 180-200 nanometers wide. But their behavior is very different.
HSV-1 was first isolated in 1942 and was long thought to cause only oral infections. It’s the main reason you get cold sores on your lips. But today, it’s responsible for 30-50% of new genital herpes cases in high-income countries. In fact, in North America and Europe, more young adults are getting genital herpes from HSV-1 than from HSV-2.
HSV-2, isolated in 1956, is still the classic cause of genital herpes. It prefers the sacral nerves near the lower spine and tends to reactivate more often. About 13% of people aged 15-49 have HSV-2 globally, with higher rates among women and Black populations in the U.S. (21% vs. 14% in men, 35% vs. 12% in White Americans).
Even though they share about 50% of their DNA, HSV-1 and HSV-2 don’t behave the same way. HSV-2 recurs on average 4-5 times a year. HSV-1 genital infections recur less than once a year in 75% of cases. Asymptomatic shedding - when the virus is active but you feel nothing - happens 10-20% of days with HSV-2, compared to 5-10% with HSV-1.
What Do the Symptoms Actually Look Like?
The first outbreak is usually the worst. For oral HSV-1, kids often get herpetic gingivostomatitis: fever over 38.5°C, mouth ulcers, bad breath, and trouble swallowing. About 1 in 20 kids with this need hospital care.
For genital HSV-2, symptoms hit hard: 93% of people get painful ulcers, 78% feel burning when peeing, 65% have swollen lymph nodes in the groin, and 40% get fever and muscle aches. The blisters turn into open sores, crust over, and heal in 7-21 days - no scars, but the pain can be intense.
Before the blisters appear, most people feel it coming. A tingling, itching, or burning sensation in the same spot - sometimes just for a few hours. That’s the prodrome. Recognizing this is key. Starting antivirals within 24 hours cuts healing time in half.
Recurrent outbreaks are milder. Instead of 10+ ulcers, you might get one or two small blisters. Pain drops from a 7/10 to a 4/10 on average. Many people never have a second outbreak. Others get them every few months.
Not all herpes is on the skin. HSV-1 causes 98% of herpes keratitis - a corneal infection that leads to 50,000 cases of vision loss each year in the U.S. alone. HSV-2 rarely causes this. And while rare, herpes encephalitis (brain inflammation) is almost always HSV-1. It strikes suddenly with seizures, confusion, and fever. Without treatment, half of patients die.
How Antiviral Therapy Works
There’s no cure for herpes. But antiviral drugs stop the virus from multiplying. They don’t kill it - it stays hidden in your nerves for life. But they make it far less dangerous.
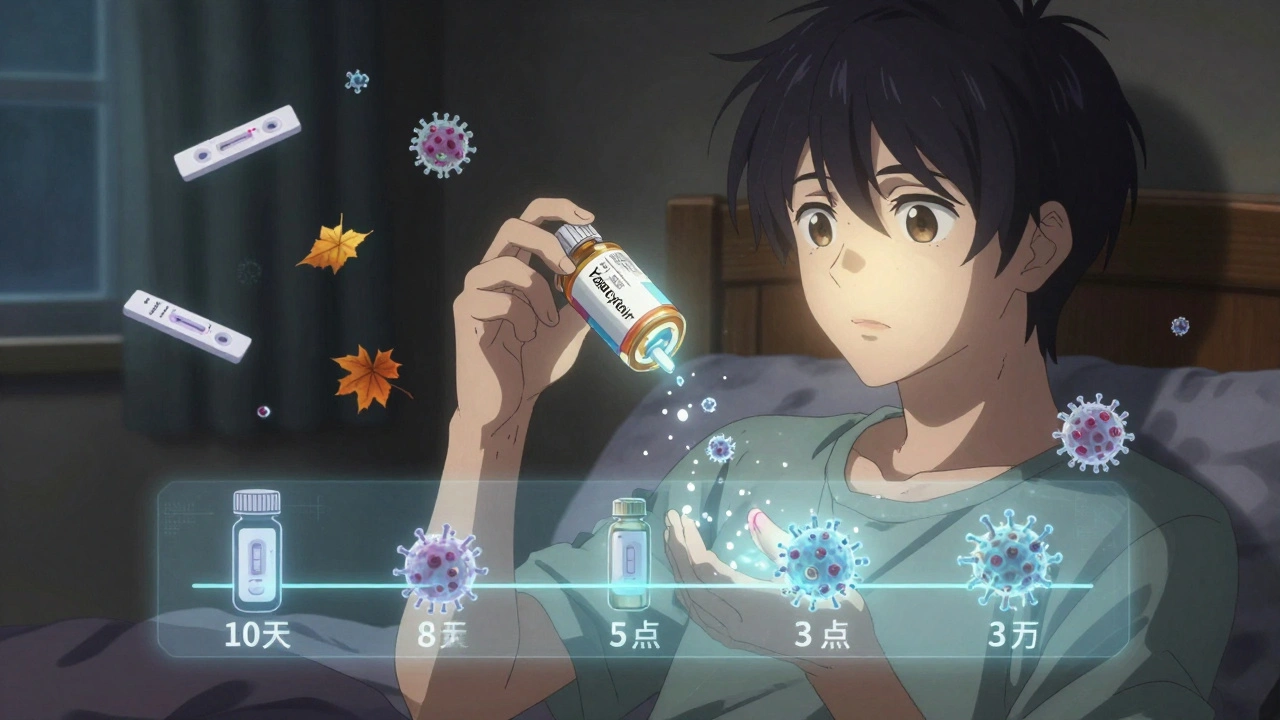
Three main drugs are used: acyclovir, valacyclovir, and famciclovir. All work the same way - they block the virus’s ability to copy its DNA. But they differ in how often you take them.
Acyclovir is the oldest. You take it 3-5 times a day. That’s hard to stick with. Valacyclovir is its prodrug - your body turns it into acyclovir. You take it just twice a day. Famciclovir is similar, often taken twice daily. For most people, valacyclovir is the go-to because it’s easier and works just as well.
For the first genital outbreak, the CDC recommends acyclovir 400mg three times daily for 5-10 days. This cuts healing time from 19 days to about 10. Pain drops from 12 days to 8. If you wait more than 72 hours to start, the benefit shrinks.
For cold sores, a single 2-gram dose of valacyclovir can shorten the outbreak by a day or two - if you catch it early.
Suppressive Therapy: Daily Prevention
If you have frequent outbreaks (six or more a year), or if you have a partner who doesn’t have herpes, daily suppressive therapy makes sense.
Valacyclovir 500mg once a day reduces transmission to uninfected partners by 48%. For HSV-2, that’s a big deal. In one study, only 2% of partners got infected over a year with daily therapy, compared to 4% without.
But it’s not for everyone. HSV-1 genital infections recur so rarely that most doctors don’t recommend daily pills. And for people with mild outbreaks, episodic treatment - taking meds only when symptoms start - works fine.
Side effects are rare. Headache and nausea are the most common. Less than 1% of people report kidney issues - usually only if they already have kidney disease or take too much.
Resistance and New Treatments
Most people respond perfectly to acyclovir. But in those with weakened immune systems - like people with HIV and CD4 counts below 100 - resistance is growing. About 10% of isolates in this group don’t respond to acyclovir.
When that happens, doctors switch to foscarnet or cidofovir. Both are given intravenously and can be harsh on the kidneys. But they work.
The big news in 2023 was the FDA approval of pritelivir. It’s a new drug that blocks a different part of the virus - the helicase-primase complex. In trials, it cut viral shedding by 87% in 48 hours, compared to 52% for foscarnet. It’s already being used for acyclovir-resistant cases.
There are also vaccines in development. GEN-003 and Simplirix showed 50% reduction in shedding in phase II trials. They’re not ready yet, but they’re a step toward prevention.

Diagnosis: What Tests Actually Tell You
Don’t rely on how it looks. Other things - like yeast infections, contact dermatitis, or even syphilis - can mimic herpes.
The gold standard is PCR testing from a swab of an active sore. It’s 95-98% accurate and gives results in 1-3 days. Viral culture is outdated - it misses up to 30% of cases.
Blood tests (serology) detect antibodies. Type-specific tests like HerpeSelect or EUROIMMUN’s recomLine HSV IgG can tell HSV-1 from HSV-2 with over 96% accuracy. But they won’t show a new infection until 12-16 weeks after exposure. If you test too soon, you’ll get a false negative.
Doctors often use both: a swab during an outbreak, then a blood test later to confirm type and rule out hidden infection.
Real Stories, Real Impact
People living with herpes face more than physical symptoms. A 2023 survey of 1,500 HSV-positive individuals found 74% felt anxiety from stigma. 45% said it hurt their relationships. One in three waited over six months to tell a partner.
But many find relief. On Drugs.com, 82% of users reported valacyclovir reduced outbreak duration from 10 days to 5. One Reddit user wrote: “First outbreak had 12 ulcers and I couldn’t pee without numbing gel. After starting daily valacyclovir, my outbreaks dropped to 1-2 small sores that last 2-3 days.”
Others switched to famciclovir because acyclovir gave them nausea. That’s normal - not every drug works for every body. Finding the right one takes trial and patience.
What You Can Do Right Now
If you think you have herpes:
- See a doctor within 24 hours of symptoms starting - timing matters.
- Ask for a PCR swab, not just a visual diagnosis.
- Get a type-specific blood test if you’re not in an outbreak.
- Ask about suppressive therapy if you have more than 4 outbreaks a year.
- Tell partners before sex - it’s not just ethical, it’s how you protect them.
If you’re already diagnosed:
- Keep antivirals on hand - don’t wait to refill.
- Track your outbreaks. What triggers them? Stress? Menstruation? Sunlight?
- Use condoms - they reduce transmission by 30-50%, even without medication.
- Don’t shame yourself. Millions live full, healthy lives with herpes.
Herpes isn’t a life sentence. It’s a manageable condition. With the right treatment, you can live without fear of outbreaks - and without fear of passing it on.
Can you get herpes from kissing?
Yes. HSV-1 spreads easily through saliva, even when there’s no visible sore. About 90% of people with oral herpes don’t know they have it. Kissing someone with an active cold sore carries high risk, but transmission can also happen during asymptomatic shedding. Using antiviral meds reduces this risk.
Can HSV-1 turn into HSV-2?
No. HSV-1 and HSV-2 are two different viruses. One doesn’t change into the other. But you can be infected with both. For example, someone with oral HSV-1 can also get genital HSV-2 through sexual contact. They’re separate infections.
Is herpes only spread during outbreaks?
No. The virus sheds without symptoms about 10-20% of days with HSV-2, and 5-10% with HSV-1. This is called asymptomatic shedding. That’s why daily antiviral therapy is so effective - it cuts shedding by up to 90%, even when you feel fine.
Can you have herpes and never know it?
Yes. Up to 80% of people with HSV-2 don’t know they’re infected. Many have mild or no symptoms. Others mistake outbreaks for yeast infections, razor burn, or ingrown hairs. Blood tests can reveal hidden infections - especially if you’ve had unexplained genital irritation or a partner was diagnosed.
Are there natural cures for herpes?
No. No supplement, herb, or diet has been proven to cure herpes or stop shedding. Lysine, zinc, or tea tree oil might help soothe sores, but they don’t reduce transmission or recurrence. Only FDA-approved antivirals - acyclovir, valacyclovir, famciclovir - have shown consistent, measurable results in clinical trials.
Can herpes affect pregnancy?
Yes. If a woman gets herpes for the first time late in pregnancy, there’s a 30-50% chance of passing it to the baby during delivery. But if she’s had it before, her body has antibodies that protect the baby. Doctors recommend suppressive therapy in the last month of pregnancy for women with frequent outbreaks. A C-section is only done if there’s an active outbreak at delivery.
How much does antiviral treatment cost?
With insurance, valacyclovir 500mg daily costs $35-$60 per month. Without insurance, it can be $300-$400. Generic acyclovir is cheaper - around $10-$20/month. Many clinics offer patient assistance programs. Some pharmacies have discount cards that bring the price down to under $15 for a 30-day supply.
Can you get herpes from a toilet seat or towels?
No. The herpes virus dies quickly outside the body - within seconds on dry surfaces. Transmission requires direct skin-to-skin contact with an infected area. You can’t catch it from toilet seats, towels, or swimming pools.
Saket Modi
December 3, 2025 AT 02:21Chris Wallace
December 3, 2025 AT 13:00william tao
December 4, 2025 AT 15:01John Webber
December 6, 2025 AT 05:46Shubham Pandey
December 7, 2025 AT 13:19Elizabeth Farrell
December 8, 2025 AT 07:15Sheryl Lynn
December 9, 2025 AT 11:06Paul Santos
December 10, 2025 AT 02:01Eddy Kimani
December 11, 2025 AT 06:12Chelsea Moore
December 11, 2025 AT 11:38