How Betamethasone Is Used to Treat Urticaria

Urticaria, commonly known as hives, shows up as raised, itchy red welts on the skin. It can come on suddenly after eating certain foods, taking medication, or even from stress or heat. For many people, antihistamines are the first line of defense. But when those don’t cut it-when the hives won’t go away for days or weeks-doctors sometimes turn to betamethasone.
What is betamethasone?
Betamethasone is a betamethasone is a synthetic corticosteroid that reduces inflammation and suppresses the immune system. It’s not a cure for urticaria, but it helps calm the body’s overactive response that causes the swelling and itching. Unlike antihistamines that block histamine, betamethasone works deeper, targeting the root of the inflammation.
It comes in several forms: cream, ointment, lotion, and injection. For urticaria, doctors most often prescribe the topical versions-applied directly to the skin. In severe, widespread cases, oral tablets or shots may be used, but only for short periods.
Why use betamethasone for hives?
Most cases of acute urticaria clear up on their own within hours or days. But chronic urticaria-lasting more than six weeks-can be exhausting. People describe it as a constant, burning itch that interferes with sleep, work, and daily life. Antihistamines help about 60% of these patients. For the rest, the next step is often a corticosteroid like betamethasone.
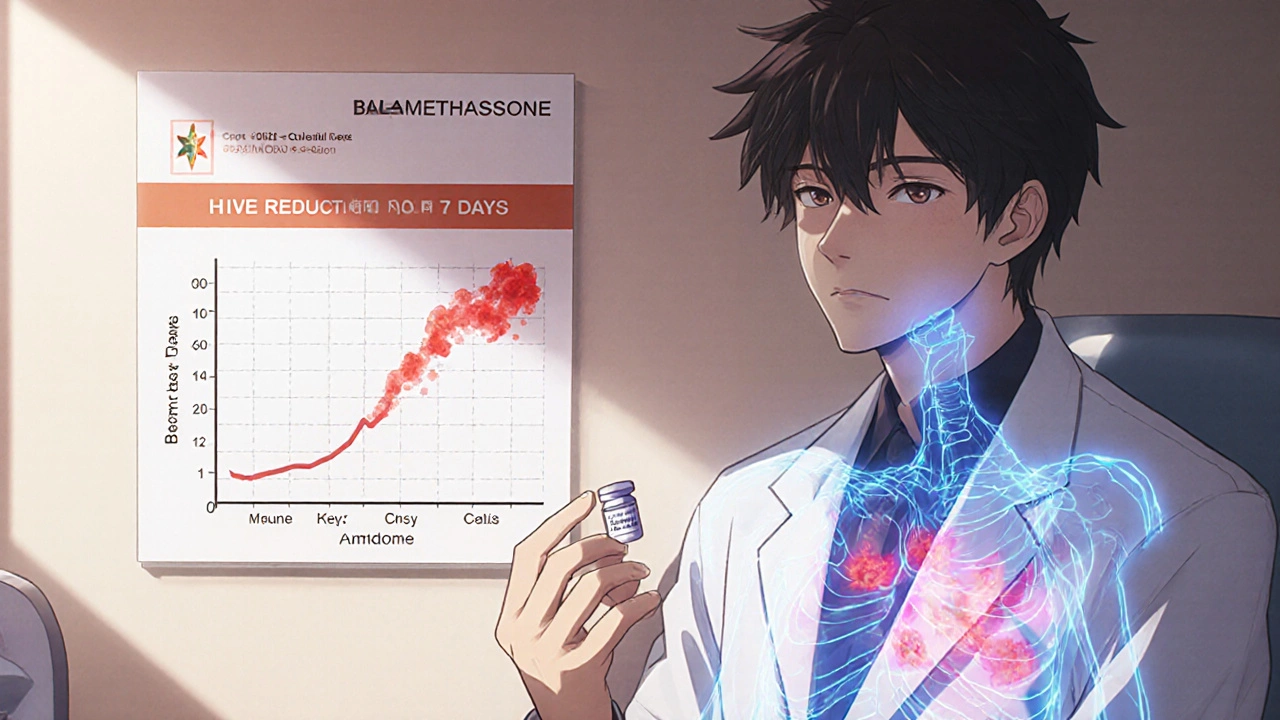
A 2023 study in the Journal of Allergy and Clinical Immunology followed 187 patients with chronic urticaria who didn’t respond to high-dose antihistamines. Half were given betamethasone tablets for seven days. Within three days, 72% reported a 50% or greater reduction in itch and hive count. By day seven, nearly 60% had near-complete clearance. That’s a big jump compared to the placebo group, where only 23% saw similar improvement.
It works fast. Most people notice less itching within 24 to 48 hours. That’s why it’s often used as a bridge-while waiting for longer-term treatments like omalizumab (an injectable biologic) to take effect.
How is it applied?
If your doctor prescribes betamethasone cream or ointment, you’ll typically apply a thin layer to the affected areas two to three times a day. Don’t rub it in hard. Just spread it gently. Use only on the hives, not on healthy skin.
For oral tablets, the usual dose is 0.5 to 1 mg once daily for 5 to 7 days. Never take it longer than your doctor says. Even a week of oral betamethasone can cause side effects like increased appetite, trouble sleeping, or mood swings. Longer use risks more serious issues: bone thinning, high blood sugar, or adrenal suppression.
Topical betamethasone is safer, but still not risk-free. Using it on large areas of skin or under occlusion (like covering it with plastic wrap) can cause the steroid to soak into your bloodstream. That’s why it’s not recommended for kids under 12 or for long-term use on the face, armpits, or groin.
When not to use betamethasone
Betamethasone isn’t for everyone. Avoid it if you have:
- An active skin infection (bacterial, fungal, or viral like herpes)
- Known allergy to corticosteroids
- Severe liver or kidney disease
- Diabetes that’s poorly controlled
- Pregnancy or breastfeeding without medical supervision
Also, don’t use it if your hives are caused by something like a drug reaction or autoimmune condition unless your doctor confirms it’s safe. In some cases, steroids can mask symptoms and delay proper diagnosis.
Side effects you should watch for
Topical betamethasone rarely causes big problems if used correctly. But possible side effects include:
- Thinning of the skin (atrophy)
- Stretch marks
- Changes in skin color
- Increased hair growth in the treated area
With oral use, side effects are more common and serious:
- Fluid retention and swelling
- High blood pressure
- Increased risk of infection
- Mood changes, anxiety, or insomnia
- Weight gain, especially around the face and abdomen
These usually go away after stopping the medication, but some, like bone density loss, can be permanent if used too long.

Alternatives to betamethasone
If betamethasone isn’t right for you, there are other options:
- Higher-dose antihistamines: Sometimes doubling or tripling the standard dose helps. Drugs like cetirizine or fexofenadine are often used this way.
- Omalizumab (Xolair): An injectable biologic approved for chronic urticaria. It targets IgE antibodies and works over weeks, not days. Many patients stay on it for months or years.
- Cyclosporine: An immune suppressant used off-label for stubborn cases. Requires blood tests to monitor kidney function.
- Leukotriene inhibitors: Like montelukast. Less effective than steroids but safer for long-term use.
Many doctors now prefer to jump straight to omalizumab for chronic cases, skipping steroids entirely. But betamethasone still has its place-especially when quick relief is needed, or when biologics aren’t covered by insurance or aren’t available.
What to expect after treatment
Even if betamethasone clears your hives, they might come back. That’s normal. Urticaria often flares again after stopping treatment. The goal isn’t always permanent elimination-it’s control. Many people learn to manage flare-ups with a combination of antihistamines and short steroid bursts.
Keep a symptom journal. Note what you ate, what you were stressed about, or what you were exposed to before a flare. Patterns often emerge. Some people find that avoiding alcohol, spicy food, or NSAIDs like ibuprofen helps reduce outbreaks.
If hives return within a week after stopping betamethasone, talk to your doctor. You may need a longer-term plan. Don’t try to restart the steroid on your own. Repeated use can lead to tolerance or adrenal issues.
Final thoughts
Betamethasone is a powerful tool-but it’s not a first-line fix for hives. It’s best used sparingly, for short periods, and only when other treatments fail. Used right, it can give you back days-or weeks-of relief from unbearable itching. Used wrong, it can cause more harm than good.
If you’re considering betamethasone for urticaria, make sure you understand why your doctor is recommending it. Ask about alternatives. Ask about risks. And never stop or restart it without medical advice. Your skin will thank you.
Can betamethasone cure urticaria?
No, betamethasone doesn’t cure urticaria. It only reduces inflammation and symptoms temporarily. Urticaria is often caused by underlying triggers like allergies, autoimmune issues, or unknown factors. Betamethasone helps manage flare-ups but doesn’t address the root cause.
Is topical betamethasone safe for long-term use on hives?
No. Long-term use of topical betamethasone can cause skin thinning, stretch marks, and changes in pigmentation. It should be limited to short courses-usually no more than 1 to 2 weeks at a time. For persistent hives, doctors recommend moving to safer long-term treatments like omalizumab or higher-dose antihistamines.
How quickly does betamethasone work for hives?
Most people notice reduced itching and fewer hives within 24 to 48 hours after starting betamethasone. Topical applications show faster local relief, while oral doses work systemically and may take a bit longer to show full effect. Maximum benefit is usually seen by day 3 to 5.
Can children use betamethasone for hives?
Topical betamethasone is rarely used in children under 12 for hives due to higher risk of skin absorption and side effects. Oral use is even more restricted and only considered in severe, life-threatening cases under close medical supervision. Pediatricians usually prefer antihistamines or other safer alternatives first.
Does betamethasone interact with other medications?
Yes. Betamethasone can interact with blood thinners, diabetes medications, antifungals, and certain antibiotics. It can also reduce the effectiveness of vaccines. Always tell your doctor about all medications and supplements you’re taking before starting betamethasone.
Shana Labed
October 31, 2025 AT 16:28OMG I JUST FOUND OUT BETAMETHASONE CAN GIVE YOU IMMEDIATE RELIEF?? I’VE BEEN DEALING WITH CHRONIC HIVES FOR 14 MONTHS AND MY DOCTOR WANTED ME TO JUST ‘TAKE ANTIHISTAMINES AND LIVE WITH IT’ 🤬 I WENT TO A DERMA SPECIALIST LAST WEEK AND THEY PRESCRIBED ME A 5-DAY COURSE-LIKE, DAY 2 I COULD SLEEP WITHOUT SCRATCHING MY ARMS BLOODY. IT’S NOT A CURE BUT IT’S LIKE A GODSENT PAUSE BUTTON FOR MY LIFE. THANK YOU FOR THIS POST!!
California Daughter
November 2, 2025 AT 09:00...I'm sorry, but... you just said 'betamethasone'... twice... in the same paragraph?... Did you even proofread this?... Also, 'synthetic corticosteroid that reduces inflammation and suppresses the immune system'... is that really the best you could do?... You didn't even mention glucocorticoid receptor binding... and you call this medical content?... 😅
Vishwajeet Gade
November 3, 2025 AT 02:54US doctors love steroids too much. In India, we use ayurvedic herbs like neem and turmeric for hives. Betamethasone? It’s like using a flamethrower to kill a mosquito. Your body gets weak. Then you need more drugs. Then you’re addicted. I’ve seen it. My cousin got diabetes after 1 week of this stuff. Stop promoting western junk.
Casey Crowell
November 3, 2025 AT 08:32Just wanted to say-this post is 🔥. I’ve been on omalizumab for 8 months now and honestly? I wish I’d known about betamethasone as a bridge earlier. I was suffering for 3 months before my biologic kicked in. The 24-48hr relief is REAL. Also, side effects? Yeah, I gained 8 lbs and had night sweats… but I could finally hug my kid without crying. Worth it. 🙌
Shanna Talley
November 5, 2025 AT 01:39It’s not about curing hives. It’s about giving people back their lives, even if just for a little while. I used to cancel plans every week because I looked like I’d been burned. Betamethasone didn’t fix me-but it let me breathe again. And that’s enough. Keep sharing this stuff. People need to know they’re not alone.
Samuel Wood
November 7, 2025 AT 00:32Actually, the pharmacokinetics of betamethasone dipropionate versus valerate are vastly different, and you’ve conflated them here-your citation is from JACI, but you didn’t specify the formulation. Also, 'topical versions-applied directly'-there’s a missing space. And you call this a medical guide? Please.
ridar aeen
November 7, 2025 AT 05:36That guy in India just said ayurveda is better. But… have you ever tried neem paste on a hive? It burns worse than the itch. And don’t get me started on turmeric staining your skin orange for weeks. Betamethasone is the only thing that got me out of bed. I’m not anti-alternative, but I’m pro-not-losing sleep.
chantall meyer
November 8, 2025 AT 17:58Most people don’t need steroids. They need to stop eating processed sugar and gluten. My hives vanished after I went paleo. Betamethasone is just a bandaid for poor lifestyle choices. If you’re relying on synthetic corticosteroids, you’re not healing-you’re masking. The body doesn’t lie.