How to Prevent Heat-Related Medication Problems in Seniors
When the temperature climbs, most people think about drinking more water or turning on the fan. But for seniors taking certain medications, heat isn’t just uncomfortable-it’s dangerous. Every year, hundreds of older adults end up in the hospital because their medications make it harder for their bodies to handle hot weather. Some of these drugs don’t just cause side effects-they can turn a warm day into a life-threatening situation.
Why Seniors Are More at Risk
As people age, their bodies change. Sweat glands don’t work as well. Thirst signals get weaker. The heart doesn’t pump blood as efficiently. These natural changes already make it harder to cool down. But when you add in medications, the risk multiplies. About 87% of seniors over 65 take two or more prescription drugs. Many of those drugs interfere with how the body manages heat and fluids.Medications That Make Heat More Dangerous
Not all medications are risky in the heat, but some are. Here are the main ones to watch for:- Diuretics (like Hydrochlorothiazide and Furosemide): These are often called "water pills" and are used for high blood pressure or heart failure. They make you pee more, which can lead to dehydration. But they also reduce your thirst by 30-40%, so you might not even realize you’re not drinking enough.
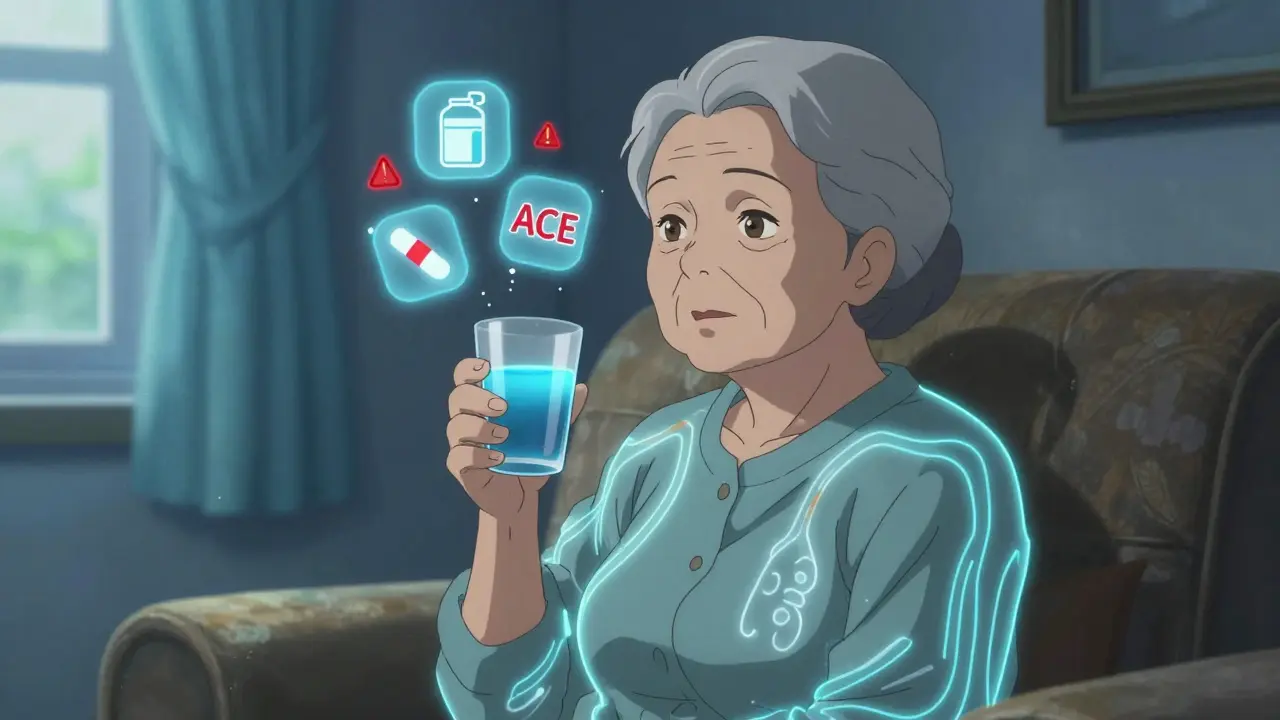
- ACE inhibitors and ARBs (like Benazepril, Losartan): These blood pressure medications can lower your thirst by about 25%. They also reduce blood volume, which makes it harder for your body to circulate blood to the skin to cool off.
- Antipsychotics (like Quetiapine, Clozapine): Commonly prescribed for dementia or mental health conditions, these drugs disrupt the brain’s thermostat. Research shows they can raise core body temperature by 1.5-2.0°F even without physical activity.
- Anticholinergics (like Benadryl, Tylenol PM): These are found in many over-the-counter sleep aids and allergy meds. They block sweat production by 35-50%. No sweat means no cooling. This is especially dangerous during a heat wave.
- Some antibiotics and antifungals: Certain drugs, like tetracycline or fluconazole, make the skin extra sensitive to sunlight. Sunburn can happen in half the time it normally would, increasing the risk of heat stress.
Worst of all, the danger grows when these drugs are taken together. A senior on a diuretic and an ACE inhibitor might lose too much sodium and fluid. Their blood pressure can drop suddenly. They might feel dizzy, fall, and break a hip. CDC data shows that 22% of heat-related falls in seniors involve these drug combinations.
What to Do: A Step-by-Step Prevention Plan
Preventing heat-related problems isn’t about guesswork. It’s about planning.- Review all medications before summer. Talk to your pharmacist or doctor. Ask: "Which of my drugs could make me more sensitive to heat?" Don’t wait until it’s hot. Do this in late spring. A 2022 study from Johns Hopkins found that seniors who had a structured medication review before summer had 37% fewer heat-related ER visits.
- Ask about adjusting doses. On very hot days, your doctor might recommend temporarily lowering a diuretic dose or skipping it for a day. Never do this without medical advice-but do ask if it’s an option.
- Check fluid restrictions. Many seniors with heart failure are told to limit fluids. But during heat waves, that can backfire. About 43% of these patients develop dangerous electrolyte imbalances when it’s hot. Ask your doctor if it’s safe to drink a little more water on hot days.
- Know your hydration targets. The National Institute on Aging recommends 8-10 eight-ounce glasses of water daily during hot weather. But if you’re on a diuretic, plain water isn’t enough. You need electrolytes. Look for drinks with 120-150 mg of sodium per 8 oz. Sports drinks can work, but avoid those with too much sugar.
- Avoid caffeine and alcohol. Both make you pee more and worsen dehydration. Coffee, tea, soda, and beer are not safe choices during heat waves.

Environmental Changes That Save Lives
Medication reviews are essential-but so is your environment.- Keep your home cool. The CDC recommends keeping indoor temperatures below 78°F (25.6°C). If you don’t have air conditioning, find a public place with AC-libraries, malls, community centers. Even a few hours a day can make a difference.
- Dress smart. Wear lightweight, loose, light-colored clothes made of cotton. Synthetic fabrics trap heat. Cotton can reduce how hot you feel by 5-7°F.
- Use sunscreen. If you’re on medications that increase sun sensitivity, you can burn in under 10 minutes. Use SPF 15 or higher, and reapply every 2 hours-or after sweating. The FDA says some drugs increase sunburn risk by 400-600%.
- Plan outings wisely. Avoid being outside between 10 a.m. and 4 p.m., when it’s hottest. If you must go out, go early in the morning or after sunset.
Signs of Trouble-Don’t Wait
Heat exhaustion and heat stroke don’t always look the same in seniors. Medications can mask the usual signs.Heat exhaustion symptoms: Heavy sweating, muscle cramps, headache, nausea, dizziness, weakness, fainting. But seniors might only show confusion or quiet fatigue. That’s because 41% of heat-exposed seniors don’t show classic symptoms, according to the NIA.
Heat stroke symptoms: Body temperature above 103°F, hot dry or damp skin, rapid pulse, confusion, loss of consciousness. This is a medical emergency. If you see these signs, call 911 immediately.
Don’t wait to see if it gets better. The CDC says 65% of heat exhaustion cases turn into heat stroke within 2-4 hours if untreated. And heat stroke can cause brain damage or death.

What Caregivers Can Do
If you care for an older adult, your role is critical.- Check in twice a day during heat waves-morning and evening. Ask: "How are you feeling?" Look for subtle changes: slurred speech, slower movement, not eating, or not answering normally.
- Use a thermometer. A simple digital one can catch rising body temperature before symptoms appear.
- Know your local resources. Many communities have cooling centers. Some offer free rides for seniors during heat alerts.
- Use the CDC’s new Heat and Medication Risk Assessment Tool (HM-RAT). It’s free, online, and lets you enter a senior’s medications to get a personalized risk score.
Programs like the American Geriatrics Society’s "I’m OK" check-in system have cut heat-related hospitalizations by 33% in senior living communities. Simple daily questions-"Are you drinking? Are you cool? Are you feeling off?"-can save lives.
What’s New in 2026
This year, things are getting better. The National Institute on Aging and the EPA launched HeatRisk.gov, a website that combines local heat forecasts with medication risk data. It’s already helping over a million seniors and their families plan ahead.Researchers are also testing a new "heat resilience" supplement designed for seniors on multiple medications. Early results show it improves the body’s ability to handle heat by 28%. It’s not available yet, but it shows how seriously this problem is being taken.
And the numbers are clear: Climate change means more extreme heat days. By 2050, the CDC predicts there will be 50% more days over 90°F than there were in 2020. That means more seniors at risk. Prevention isn’t optional anymore. It’s urgent.
Can seniors stop taking their medications during a heat wave?
No. Never stop or change a medication without talking to a doctor. Some drugs, like blood pressure or heart medications, can be dangerous if stopped suddenly. Instead, ask your doctor if the dose can be adjusted temporarily or if there’s a safer alternative for hot weather.
Is it safe for seniors to use fans during heat waves?
Fans only move hot air around-they don’t cool the body. If the temperature is above 90°F, fans won’t help much, especially for seniors on medications that reduce sweating. Air conditioning is the only reliable way to lower body temperature safely.
What’s the best way to hydrate if I’m on a diuretic?
Drink water regularly, but also include electrolyte drinks with 120-150 mg of sodium per 8 oz. Avoid sugary sports drinks. If you’re unsure, ask your pharmacist for a list of safe options. Some brands make low-sugar, high-electrolyte drinks specifically for older adults.
Do over-the-counter meds like Benadryl really increase heat risk?
Yes. Benadryl and similar anticholinergics block sweat, which is your body’s main cooling system. Even one dose can reduce sweating by up to 50%. Many seniors take them for sleep or allergies without realizing the danger. Switch to non-drowsy allergy meds like loratadine, and use sleep aids only if approved by a doctor.
How do I know if my loved one is overheating?
Look for subtle signs: confusion, quietness, not eating, dizziness, or unusual fatigue. They might not say they feel hot. Their skin might be dry and hot to the touch, or they might be sweating more than usual. Take their temperature if you can. If it’s above 100.4°F and they’re acting off, seek help immediately.
Are heat-related medication problems preventable?
Yes. Studies show that with a medication review, proper hydration, cooling strategies, and caregiver check-ins, heat-related hospitalizations can drop by over 30%. This isn’t just about comfort-it’s about survival. The tools and knowledge exist. What’s needed now is action.
Next Steps for Families and Seniors
Start today. Make a list of every medication-prescription, over-the-counter, and supplements. Bring it to your next doctor or pharmacist visit. Ask: "Which of these could be dangerous in hot weather?" Write down their answers. Then, make a simple plan: cool place to go, water and electrolyte drinks on hand, check-in schedule, emergency number posted by the phone.Heat doesn’t care if you’re old or sick. But with the right information and preparation, you can protect yourself-or someone you love-from a danger that’s entirely preventable.
Juan Reibelo
January 25, 2026 AT 01:07Wow. This is the most important thing I’ve read all year. I didn’t realize my grandpa’s blood pressure meds could turn a 90-degree day into a death sentence. I’m printing this out and taking it to his doctor next week. Thank you for writing this.
Viola Li
January 26, 2026 AT 19:28Actually, this whole article is fearmongering. Seniors have been fine for decades without this level of panic. Maybe they just need to stop being so fragile? I’ve seen 80-year-olds work in fields in 100-degree heat-no meds, no AC, no problem.
venkatesh karumanchi
January 27, 2026 AT 18:09Thank you for sharing this. In India, we see this every summer-elders on diuretics drinking less because they think it’s ‘bad for the kidneys.’ But they don’t know sweat is their only cooling system. I’ve told my aunt to keep electrolyte packets by her bed now. Small changes, big difference.
Jenna Allison
January 29, 2026 AT 14:03As a geriatric pharmacist, I can confirm every single point here. Anticholinergics are the silent killers. Benadryl is literally a heat-risk drug. I’ve seen patients on 50mg of diphenhydramine daily-no one tells them it blocks sweating. We need mandatory counseling when these are prescribed to seniors. This isn’t just advice-it’s clinical necessity.
Kat Peterson
January 30, 2026 AT 04:08OMG I’m crying 😭 I just realized my mom’s ‘sleep aid’ is basically a heat bomb! I’ve been giving her Tylenol PM for years because she ‘just needs a little help.’ I’m so guilty. I’m switching her to melatonin TODAY. This article just saved her life. 🙏 #HeatAwareness
Shelby Marcel
January 31, 2026 AT 02:00wait so benadryl makes you not sweat?? like… the stuff i take for my allergies?? i thought it just made me sleepy… this is wild. i gotta check my meds lol
blackbelt security
February 1, 2026 AT 17:13Prevention is the ultimate win. This isn’t about being scared-it’s about being smart. Get the list. Talk to the doc. Know the signs. You’re not just protecting someone-you’re giving them back their independence. Do the work. It’s worth it.
Patrick Gornik
February 2, 2026 AT 14:10Let’s deconstruct the epistemology of thermal regulation in geriatric pharmacology. The body’s thermoregulatory apparatus-once a symphony of homeostatic equilibrium-is now a fragile orchestra conducted by polypharmacy. The pharmaceutical-industrial complex, in its infinite wisdom, has weaponized the very mechanisms meant to sustain life. We are not merely managing heat-we are negotiating a biochemical betrayal engineered by corporate profit margins and clinical inertia. The real crisis? We’ve normalized death as a side effect.
Luke Davidson
February 3, 2026 AT 17:38I lost my uncle last summer. He didn’t say a word. Just sat in his chair, quiet. We thought he was tired. Turns out his heart meds + diuretic + Benadryl for allergies turned a simple afternoon into a nightmare. I wish I’d known this. Please, if you’re reading this-ask your loved ones about their meds. Don’t wait for a tragedy. Talk now.
Shanta Blank
February 4, 2026 AT 03:55Of course this is a problem. The system is designed to keep seniors medicated, not alive. Pharma companies don’t care if you sweat or not-they care if you refill. And the doctors? Too busy to care. This article is just a Band-Aid on a hemorrhage. We need systemic change-not ‘tips’ for surviving the machine.
Kevin Waters
February 4, 2026 AT 23:52Great breakdown. I’ve been telling my mom to stop drinking soda in the heat, but I didn’t realize her blood pressure med was the real culprit. I just scheduled her pharmacy consult for next Tuesday. And I’m buying her a cheap digital thermometer. Small steps, but they matter.
Jamie Hooper
February 5, 2026 AT 21:31bloody hell i just checked my nan’s meds and she’s on furosemide AND benadryl… she’s been taking that for ‘nerves’ since 2018. i’m calling the GP first thing monday. thanks for the wake up call mate 🙏
Husain Atther
February 6, 2026 AT 12:08This is a thoughtful and necessary guide. In many cultures, elders are expected to endure discomfort silently. But science shows us that this silence is not strength-it is vulnerability. Let us listen, learn, and act-not with pity, but with dignity.