Hyperpigmentation: Understanding Melasma, Sun Damage, and Effective Topical Treatments

When your skin starts showing dark patches-on your cheeks, forehead, or hands-it’s easy to assume it’s just a tan that won’t fade. But if those spots don’t go away after summer, or if they keep coming back no matter how much sunscreen you use, you’re likely dealing with hyperpigmentation. Not all dark spots are the same. Two of the most common types, melasma and sun damage, look similar but behave completely differently. Treating them the same way can make things worse. Understanding the difference isn’t just helpful-it’s essential.
What’s Really Causing Your Dark Patches?
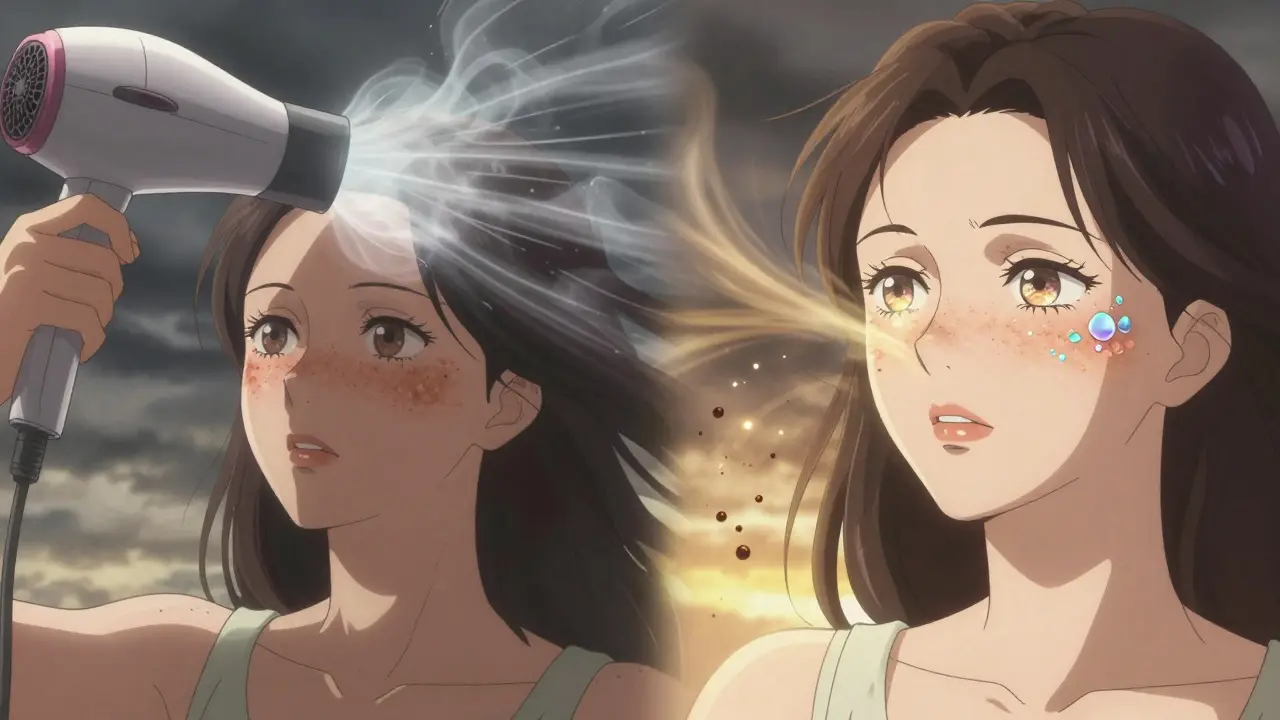
Melasma shows up as large, irregular patches, usually on the face. It’s symmetrical-both cheeks darken together, or the forehead and upper lip. It’s most common in women, especially those with medium to dark skin tones (Fitzpatrick III-VI). Hormones play a big role: pregnancy, birth control pills, or hormone replacement therapy can trigger it. Even visible light from windows or screens can make it worse. Heat, like from a hot shower or a hairdryer held too close, can also activate melanocytes-the cells that make pigment.
Sun damage, or solar lentigines, looks different. These are smaller, well-defined spots-like freckles that got bigger. They show up where the sun hits most: face, hands, shoulders. They’re caused by years of UV exposure. The more sun you’ve had over time, the more likely you’ll see them. Around 90% of fair-skinned people over 60 have them. Unlike melasma, they don’t respond to hormones. They’re purely a result of sun exposure.
Here’s the key difference: melasma is a reaction to multiple triggers-UV, visible light, heat, hormones. Sun damage is just UV. That’s why treating them the same way often fails.
Why Sunscreen Alone Isn’t Enough
Most people think SPF 30+ is enough. It’s not. Standard sunscreens block UV rays, but melasma is also triggered by visible light-blue and green wavelengths that pass right through regular sunscreen. That’s why many patients still get worse even when they "do everything right."
For melasma, you need mineral sunscreen with zinc oxide or titanium dioxide-and crucially, iron oxides. Iron oxides block visible light. A study showed that visible light contributes to 25-30% of melasma cases. Without iron oxides, you’re leaving a major trigger wide open.
And it’s not just outdoors. UV and visible light penetrate windows. If you sit near a sunny window at home or in the car, you’re still exposing your skin. Dermatologists now recommend daily sunscreen even when you’re indoors if you have melasma.
Topical Treatments That Actually Work
Not all creams are created equal. Here’s what’s backed by clinical data:
- Hydroquinone (4%): The gold standard for melasma. It blocks the enzyme tyrosinase, which makes melanin. Used alone, it helps about 30-40% of users. But when combined with tretinoin and a corticosteroid (a triple combo), success jumps to 50-70% in 12 weeks. The catch? Don’t use it longer than 3 months. Overuse can cause ochronosis-a rare but permanent brownish discoloration.
- Tretinoin (0.025-0.1%): This retinoid speeds up skin cell turnover. It doesn’t lighten pigment directly, but it helps push melanin out of the skin faster. Used every other night, it boosts the effect of hydroquinone and reduces irritation.
- Vitamin C (10-20% L-ascorbic acid): A powerful antioxidant. It neutralizes free radicals from UV and visible light, and it also inhibits tyrosinase. It’s gentle, safe for long-term use, and great for daily prevention.
- Tranexamic acid (5%): Originally a blood thinner, it’s now used topically to block pigment signals from skin cells. In clinical trials, it reduced melasma by 45% in 12 weeks with no major side effects.
- Cysteamine cream (10%): A newer option showing 60% improvement in melasma after 16 weeks. It’s less irritating than hydroquinone and doesn’t carry the same long-term risks.
For sun damage, hydroquinone helps-but it’s not the best option. Lasers and light treatments work faster and more predictably. Topicals are fine for maintenance, but if you want quick results, energy-based devices are the way to go.

Laser and Light Treatments: When They Help and When They Hurt
IPL (Intense Pulsed Light) is great for sun damage. It targets the pigment, heats it up, and the skin sheds it in a few days. Most people see results in 1-2 sessions. But for melasma? IPL is risky. The heat can trigger more pigment production. Studies show a 30-40% chance of making melasma worse.
Some dermatologists use low-energy lasers like Q-switched Nd:YAG for melasma, but only after 8-12 weeks of topical suppression. This is called a "melanocyte rest" protocol. It calms down the pigment cells first, so the laser doesn’t overstimulate them. Done right, recurrence drops from 60% to 25%.
Chemical peels-glycolic, lactic, or TCA-can help too. But they’re not for everyone. In darker skin tones (Fitzpatrick IV-VI), peels carry a 25% risk of causing post-inflammatory hyperpigmentation (PIH), which is even harder to treat than melasma.
Why Melasma Keeps Coming Back
Melasma isn’t cured-it’s managed. Studies show 95% of people see it return within 6 months of stopping treatment. That’s not failure. That’s biology.
Why? Because the triggers never go away. Hormones fluctuate. The sun still rises. Visible light still streams through windows. Without daily protection and maintenance, pigment cells wake back up.
This is why long-term skincare isn’t optional. It’s the foundation. Even after your skin clears, you need to keep using sunscreen with iron oxides, vitamin C, and maybe a low-dose retinoid or tranexamic acid every night.
The Biggest Mistake Patients Make
It’s not using the wrong cream. It’s not skipping treatments. It’s not even missing appointments.
It’s sunscreen application.
Most people use less than half the amount they should. For the face and neck, you need about a quarter teaspoon-roughly the size of a nickel. And you have to reapply every 2 hours if you’re outside. Most people don’t. A clinical survey found 70% of patients with melasma fail to reapply or use enough. That’s why their treatment stalls.
Also, many start with over-the-counter products-niacinamide, kojic acid, licorice root extracts. These are safe and mild, but they rarely move the needle on melasma. They’re good for prevention or maintenance, but not for clearing stubborn patches.
What Works Best Together
The most effective approach is layered:
- Morning: Vitamin C serum → mineral sunscreen with iron oxides (SPF 50+)
- Evening: Alternate nights: hydroquinone (4%) one night, tretinoin (0.05%) the next. Skip both one night a week to let skin recover.
- Every 4-6 weeks: Gentle chemical peel (if skin type allows)
- Once skin is stable: Consider laser or light therapy, but only after 3 months of consistent topicals
This combo is used by 75% of dermatologists today for moderate melasma-up from 45% just five years ago. It’s not flashy. It’s slow. But it works.
Who’s Most Affected-and Why
Melasma hits Black, Asian, and Hispanic women 3-5 times more often than Caucasian women. That’s not because they tan more. It’s because their skin has more active melanocytes, and those cells are more sensitive to hormones and light.
Post-inflammatory hyperpigmentation (PIH) is another common issue, especially in darker skin. It shows up after acne, eczema, or even a scratch. It’s not sun-related. Lasers often make PIH worse. Topicals are safer and more effective here too.
And cost? It adds up. Prescription topicals run $50-$150 a month. A single laser session is $300-$600. Many patients delay seeing a dermatologist because they try OTC products first. But by the time they get help, the condition is deeper and harder to treat.
What’s Changing in 2025
The FDA is considering reclassifying hydroquinone from prescription-only to over-the-counter-but with strict safety labeling. That could make it more accessible, but also riskier if used incorrectly.
New agents are emerging: cysteamine, tranexamic acid, and even oral tranexamic acid for severe cases. Genetic testing is on the horizon. Dermatologists believe that within five years, we’ll be able to test a patient’s skin cells to predict which treatment will work best for them-personalized pigmentation therapy.
For now, the best advice hasn’t changed: protect your skin from UV and visible light, use proven topicals consistently, and don’t rush into lasers without a plan.
Hyperpigmentation isn’t a flaw. It’s a signal. Your skin is reacting to something. Listen to it. Treat it right. And don’t give up-because with the right approach, you can get your skin back.
Is melasma the same as sun spots?
No. Melasma appears as large, symmetrical patches on the face, often triggered by hormones and visible light. Sun spots (solar lentigines) are smaller, scattered spots caused by UV exposure over time. They look similar but need different treatments. Lasers work well for sun spots but can worsen melasma.
Can I treat melasma with over-the-counter products?
Mild cases might improve with OTC products like niacinamide, kojic acid, or vitamin C. But for noticeable melasma, prescription topicals like hydroquinone, tretinoin, or tranexamic acid are far more effective. Most patients who only use OTC creams see little to no improvement after 3-4 months.
Do I need sunscreen if I’m indoors?
Yes-if you have melasma. Visible light from windows, LED lights, and screens can trigger pigment production. Use a mineral sunscreen with iron oxides daily, even if you’re inside. Regular chemical sunscreens don’t block visible light.
How long does it take to see results from topical treatments?
You’ll usually start seeing improvement in 6-8 weeks, but full results take 3-6 months. Melasma responds slowly because it’s not just surface-level pigment-it’s a reaction deep in the skin. Patience and consistency are critical.
Why does my melasma get worse in summer?
Sun exposure increases UV and visible light, which activate melanocytes. Heat also plays a role-hot weather, saunas, or even hot showers can trigger flare-ups. That’s why strict sun protection and avoiding heat exposure are part of the treatment plan.
Can laser treatments cure melasma?
No. Lasers can improve melasma, but they don’t cure it. Without ongoing sun protection and maintenance, melasma almost always returns. Lasers are best used after topicals have calmed the skin, and even then, they’re a supplement-not a solution.
What’s the safest long-term treatment for melasma?
A daily routine of vitamin C serum and mineral sunscreen with iron oxides, plus periodic use of tranexamic acid or low-dose tretinoin. These are non-irritating, safe for years, and prevent recurrence. Hydroquinone should be used in cycles, not continuously.
Mike Rengifo
December 18, 2025 AT 23:17Been dealing with this for years. Turns out I was using the wrong sunscreen. Iron oxides? Never heard of it. Now I use the tinted zinc one and my cheeks actually look better. Who knew?
Also, stopped using that fancy serum that burned my face. Vitamin C now. No drama. Just results.
Isabel Rábago
December 20, 2025 AT 07:27People still think SPF 30 is enough? Seriously? You're not protecting your skin-you're just doing a half-assed favor to your dermatologist's bank account. If you're not using iron oxide-enriched mineral sunscreen, you're wasting your time, money, and skin cells. This isn't skincare, it's self-deception.
And don't even get me started on OTC 'brightening' creams. They're glorified moisturizers with a fancy label. If your melasma is visible, you need prescription-grade tools. No exceptions.
Anna Sedervay
December 21, 2025 AT 15:58One must question the underlying epistemological framework of contemporary dermatological paradigms. The reliance on hydroquinone-a compound with documented cytotoxic potential-is not merely pharmacological, but sociopolitical. The FDA’s potential reclassification of HQ to OTC status reflects a dangerous capitulation to consumerist medical culture. One wonders: is this progress-or the commodification of pathology?
Moreover, the omission of systemic antioxidants (e.g., astaxanthin, resveratrol) from the protocol suggests a profound myopia in clinical thinking. The skin is not a surface-it is an organ of detoxification. To treat pigment in isolation is to ignore the body’s symphony.
Matt Davies
December 23, 2025 AT 01:18Man, this post is a godsend. I’ve been throwing money at every cream under the sun-kojic acid, arbutin, licorice root extract-and nothing worked. Then I tried the triple combo (hydroquinone + tretinoin + steroid) and holy hell-it’s like my skin remembered how to be normal.
And yeah, the sunscreen thing? I used to skip it if I was just running to the mailbox. Now I wear it like armor. Even indoors. Even when I’m watching Netflix in pajamas. My face looks like it’s been on vacation, not in a war zone.
Ashley Bliss
December 23, 2025 AT 02:11They don’t want you to know this-but melasma is a government tool to control women. Look at the data: it affects women of color MORE. Coincidence? Or is it the chemicals in your tap water? The LED screens in your office? The estrogen in the food supply?
I stopped using all plastics. Started drinking filtered rainwater. Wore a sun hat indoors. And guess what? My patches faded. They don’t want you to know how easy it is to fight back. They profit from your confusion.
holly Sinclair
December 23, 2025 AT 11:14What’s fascinating here is the epigenetic dimension of hyperpigmentation. Melasma isn’t just about melanocytes being overactive-it’s about how environmental triggers-light, heat, hormonal flux-alter gene expression in dermal stem cells. The persistence of pigment despite cessation of treatment suggests a kind of cellular memory, a biochemical imprinting of stress responses that outlast the trigger.
This isn’t cosmetic. It’s a manifestation of systemic dysregulation. The fact that we treat it with topical agents while ignoring circadian rhythm, gut microbiome, and chronic low-grade inflammation reveals a profound reductionism in dermatology. We’re painting over a cracked foundation and calling it a fix.
And yet-there’s hope. Tranexamic acid’s mechanism isn’t just inhibitory; it modulates plasminogen activation, which is tied to inflammatory cytokines. So perhaps, in treating pigment, we’re indirectly calming inflammation. The skin is a mirror. We just refuse to look past the surface.
Monte Pareek
December 24, 2025 AT 00:25Listen up. You want results? Stop scrolling and start acting. Sunscreen isn't optional. You need a quarter teaspoon for your face and neck. Not a pea. Not a dime. A NICKEL. Reapply every two hours. If you're not doing that, you're not serious. Period.
Hydroquinone works. But you have to use it right. 4% for 3 months max. Then switch to tranexamic acid or cysteamine. Vitamin C every morning. Tretinoin every other night. No excuses. No OTC junk. You think your $20 cream from Target is gonna fix this? It's not a miracle. It's a marketing scam.
Lasers? Only after you've done the groundwork. Otherwise you're just burning money and making it worse. This isn't magic. It's discipline. And discipline beats luck every time.
And if you're a woman of color? You're not broken. You're just more sensitive. That means you need better tools. Not less. More. So get your act together. Your skin deserves it.
Allison Pannabekcer
December 24, 2025 AT 00:55Thank you for writing this. I’ve been so frustrated trying to figure out why my spots came back after laser. I thought I failed. Turns out I just didn’t know the difference between melasma and sun damage.
I’m going to try the vitamin C + iron oxide sunscreen combo. I’ve been using that cheap chemical SPF and wondering why nothing stuck. Maybe I just needed to listen to my skin instead of the influencers.
Also, I’m not alone in this. That’s comforting.
Sarah McQuillan
December 25, 2025 AT 06:27Interesting how everyone’s obsessed with ‘melasma’ like it’s some exotic disease. In my country, we just call it ‘sun spots’ and use lemon juice. Works fine. Why do Americans need 5-step regimens and $150 creams? Maybe if you spent less time worrying about your skin and more time getting sunlight, you’d be healthier overall.
Also, iron oxides in sunscreen? Sounds like corporate overengineering. Next they’ll tell us to wear UV-blocking pajamas.
Aboobakar Muhammedali
December 25, 2025 AT 09:48My mother had this since she was 30. She never used fancy creams. Just coconut oil and stayed in shade. Now at 70, her face is calm. Maybe the answer is not more products but less stress. Less screen. Less heat. Less hurry.
I tried the hydroquinone. Burned my skin. Stopped. Now I use vitamin C and sleep early. Slow. But my skin is quiet now. Not angry. Maybe peace is the real treatment.
anthony funes gomez
December 26, 2025 AT 16:45While the clinical efficacy of hydroquinone as a tyrosinase inhibitor is well-documented, the underlying assumption-that melanin production is a pathological endpoint to be suppressed-is ontologically problematic. Pigmentation is a biological adaptation, not a defect. The current paradigm pathologizes natural phenotypic variation under the guise of ‘cosmetic improvement.’
Moreover, the emphasis on topical agents ignores neuroendocrine modulation of melanogenesis-cortisol, ACTH, and even serotonin receptors in keratinocytes play modulatory roles. The reductionist ‘topical fix’ approach is a symptom of biomedical reductionism.
Furthermore, the proposed protocol lacks a discussion of circadian rhythm disruption as a potential driver of melanocyte hyperactivity. Blue light exposure post-sunset elevates melanin synthesis independently of UV. This is omitted. Why?
Laura Hamill
December 26, 2025 AT 22:16THEY’RE LYING TO US!! 😡
Hydroquinone is banned in Europe but they’re pushing it here? WHY? BECAUSE BIG SKINCARE WANTS YOU ADDICTED!!
I tried the triple combo and my face turned DARKER 😭 I knew it!! They’re testing it on us!!
Switched to apple cider vinegar toner and now I’m glowing 🌈✨ #FreeSkin #StopBigDermatology
William Storrs
December 27, 2025 AT 22:29You got this. I know it feels overwhelming, but you’re not starting from zero-you’re starting from awareness. That’s huge.
Just pick one thing. Maybe the sunscreen. Just that. Do it every morning for 30 days. No excuses. Then add vitamin C. Then maybe tretinoin. Slow and steady wins the race.
Your skin isn’t your enemy. It’s your ally. It’s just trying to protect you. Meet it halfway.
James Stearns
December 28, 2025 AT 05:01It is, regrettably, a matter of public record that the contemporary dermatological establishment has been complicit in the commodification of aesthetic insecurity. The proliferation of so-called ‘melasma protocols’ is not a triumph of medical science, but rather a manifestation of late-stage capitalist pathology.
One cannot help but observe that the recommended regimen-replete with proprietary formulations, expensive devices, and frequent clinical visits-serves primarily to enrich the pharmaceutical-industrial complex, while the patient is left burdened with financial strain and psychological distress.
Moreover, the suggestion that visible light warrants iron oxide supplementation is not merely a dermatological insight-it is a tacit admission that the regulatory framework governing sunscreen efficacy is fundamentally inadequate. One must ask: who benefits from this obfuscation?
Mike Rengifo
December 29, 2025 AT 14:11Wait, you’re telling me I’ve been using sunscreen wrong this whole time? I thought I was doing good. Guess I just needed someone to say it straight.
Thanks for the kick in the pants. Going to buy that zinc oxide one tomorrow.