Rechallenge After Statin-Induced Myopathy: Safe, Proven Strategies
Statin Rechallenge Risk Calculator
Use this clinical tool to assess your likelihood of successfully restarting statins after muscle symptoms.
SAMS-CI Assessment
The Statin-Associated Muscle Symptom Clinical Index helps determine your risk of successful rechallenge.
When muscle pain hits after taking a statin, it’s hard not to panic. You’ve been told these pills save lives-prevent heart attacks, reduce strokes-but now your legs ache, your shoulders feel heavy, and your doctor says to stop. You do. And then comes the real question: Can you ever take one again? The answer isn’t yes or no. It’s a step-by-step process, backed by science, and used successfully by thousands. Many people think once you have muscle pain on a statin, you’re done for good. That’s not true. With the right approach, 60 to 80% of people who stop statins due to muscle symptoms can get back on them safely. This isn’t guesswork. It’s a protocol.
What Exactly Is Statin-Induced Myopathy?
Statin-induced myopathy isn’t one thing. It’s a spectrum. At the mild end, you might feel general muscle soreness-like you’ve overdone it at the gym-without any lab changes. That’s often called myalgia. At the severe end, you get rhabdomyolysis: muscle cells breaking down, spilling proteins into your blood, and risking kidney failure. That’s rare-less than 1 in 1,000 people. But even the mild forms can scare people off statins for good.
The term Statin-Associated Muscle Symptoms (SAMS) was created in 2014 to describe muscle complaints during statin use-not automatically blaming the drug. Why? Because in double-blind trials where people didn’t know if they were taking a statin or a sugar pill, about 5% of both groups reported muscle pain. That suggests something else is going on. Maybe it’s aging. Maybe it’s another medication. Or maybe it’s the nocebo effect: the brain expecting pain, so it feels pain.
Why Rechallenge Matters
Stopping statins isn’t harmless. A 2022 review found that even a four-week break can destabilize plaques in your arteries. For someone who’s had a heart attack, stroke, or has diabetes with high cholesterol, going off statins is like turning off a fire alarm while the building is still smoking. The Cardiovascular risk (ASCVD) doesn’t wait. Rechallenge isn’t about being stubborn-it’s about survival.
Here’s the hard truth: 73% of patients who stop statins due to muscle pain are never offered a plan to try again. That’s a gap in care. You don’t have to live without statins. There are safe, structured ways to get back on them.
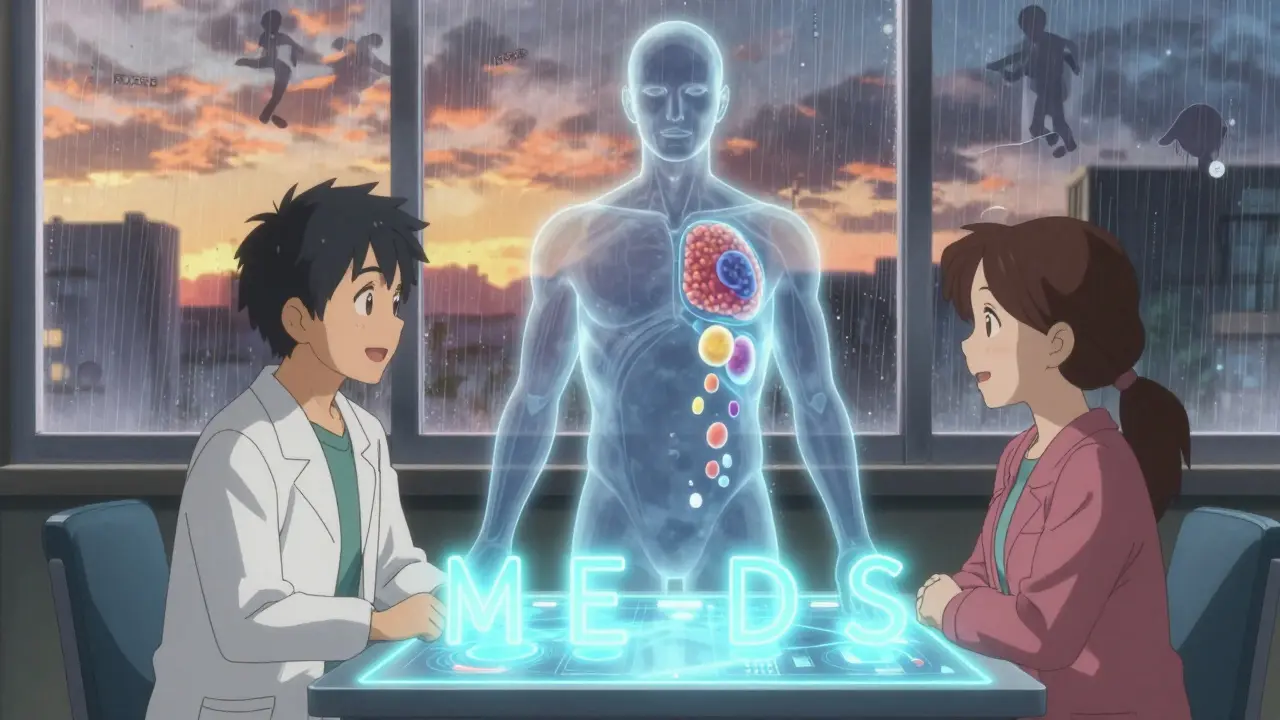
The MEDS Approach: Your Blueprint for Rechallenge
The MEDS approach is the gold standard. It’s not a theory. It’s used in lipid clinics across North America and Europe. Each letter stands for a step:
- Minimize time off statins: Don’t wait months. If symptoms are gone, restart within 2-4 weeks. Waiting too long increases your heart risk.
- Educate: Understand what’s likely real and what’s not. Learn about the nocebo effect. Know that mild soreness doesn’t mean danger.
- Diet and nutraceuticals: Reduce your statin dose by lowering your LDL another way. Add soluble fiber (oats, psyllium), plant sterols, or omega-3s. These can lower cholesterol by 10-15%, letting you use a lower, gentler statin dose.
- Systematic monitoring: Check creatine kinase (CK) levels before and 2-4 weeks after restarting. Track muscle symptoms daily. Don’t ignore new pain.
This isn’t just theory. A 2021 study of over 1,200 patients found that using MEDS led to successful rechallenge in 62% of cases. That’s more than half.
Choosing Your Rechallenge Strategy
Not all statins are the same. Some are more likely to cause muscle issues. Here’s what works:
- Switch statins: If you had trouble with simvastatin or atorvastatin, try pravastatin or fluvastatin. They’re less likely to build up in muscle tissue. In one survey, 41% of people who restarted successfully switched to one of these.
- Lower the dose: Cut the dose in half. If you were on 40 mg, try 20 mg. If you were on 80 mg, go to 10 mg. Lower doses cut muscle risk dramatically.
- Try every-other-day dosing: Instead of daily, take it every 48 hours. Studies show this maintains LDL control for most people while reducing muscle exposure. About 29% of successful rechallenges used this method.
- Avoid drug interactions: Never restart statins if you’re taking gemfibrozil, certain antibiotics (like clarithromycin), or high-dose niacin. These raise statin levels dangerously. Check every new medication with your pharmacist.
Also, check your thyroid. Low thyroid function can cause muscle pain that looks like statin side effects. Get a TSH test before restarting.
The SAMS-CI Tool: Know Your Risk Before You Restart
Not everyone needs the same approach. The Statin-Associated Muscle Symptom Clinical Index (SAMS-CI) is a 6-question tool developed by the National Lipid Association. It scores your risk of true statin intolerance. A score below 5 means you have a 91% chance of tolerating a statin again. That’s huge. It’s not magic-it’s data.
Doctors can use this to avoid unnecessary fear. If your score is low, you’re a good candidate for rechallenge. If it’s high, your doctor might skip straight to alternatives.
When NOT to Rechallenge
There are two red flags where you should NEVER try statins again:
- Rhabdomyolysis: If your CK level was more than 40 times the upper limit of normal, you had a serious muscle breakdown. Restarting is dangerous. The American Heart Association says: “Withdraw the statin and do not administer it in the future.”
- Immune-mediated necrotizing myopathy: This is rare but serious. It’s confirmed by a blood test for anti-HMGCR antibodies. If positive, your immune system is attacking your own muscle. Statins triggered it, and restarting will make it worse. You need immunosuppressants-not more statins.
If either of these happened, your doctor should have tested for them. If they didn’t, ask for a repeat test. Don’t assume it’s just muscle soreness.
Alternatives When Statins Don’t Work
If rechallenge fails, you’re not out of options. But they’re not equal.
- PCSK9 inhibitors (evolocumab, alirocumab): These are injectable drugs that lower LDL by 50-60%. They cut heart attacks and strokes by 15-17% in high-risk patients. But they cost $5,850 a month. Insurance often requires proof of statin intolerance before covering them.
- Ezetimibe: A pill that blocks cholesterol absorption. Lowers LDL by 15-20%. It’s cheap, safe, and works well with low-dose statins. Often used as a bridge.
- Bempedoic acid: A newer oral drug that lowers LDL by 20-25%. It’s less likely to cause muscle pain than statins. Approved for people who can’t tolerate statins.
Here’s the reality: statins are still the best value. A generic statin costs $4-$10 a month. PCSK9 inhibitors cost over 500 times more. If you can get back on a statin-even a low dose-you’re getting far better protection for far less money.
What Patients Really Say
Real experiences matter. On forums like the American Heart Association Support Network, 62% of people who tried rechallenge succeeded. Common success stories:
- “Switched from simvastatin 40mg to pravastatin 10mg. No pain. Kept going for 2 years.”
- “Did every-other-day dosing. My muscle pain vanished. My cholesterol stayed down.”
- “My doctor used the SAMS-CI. Said I had a 90% chance. I restarted on 10mg atorvastatin. Worked.”
But others aren’t so lucky:
- “Tried three statins at lowest doses. Still had pain. Now on evolocumab.”
- “They restarted me too fast. My legs locked up. I had to go to the ER.”
The difference? Structure. People who succeeded had a plan. Those who failed were rushed or given no options.
What You Should Do Now
If you’ve stopped a statin due to muscle pain:
- Wait 2-4 weeks after symptoms fully disappear.
- Ask for a CK blood test and a thyroid panel (TSH).
- Ask your doctor to calculate your SAMS-CI score.
- Request a switch to pravastatin or fluvastatin at half your previous dose.
- Ask about adding ezetimibe or fiber supplements to help lower your dose further.
- Monitor symptoms daily. Call your doctor if pain returns or worsens.
If your doctor says, “Just stay off statins,” ask for a referral to a lipid specialist. These protocols are standard in specialized clinics-85% of them use formal rechallenge plans. Primary care? Only 43% do.
Future Directions
Genetics are changing the game. A gene called SLCO1B1 affects how your body clears statins. The *5 variant means your body holds onto simvastatin longer-increasing muscle risk by 222%. Testing for this isn’t routine yet, but it’s coming. The FDA already notes this risk on simvastatin labels.
Future rechallenges may include genetic screening, digital symptom trackers, and AI tools that predict your risk based on your history. But today, the tools we have-MEDS, SAMS-CI, dose switching-are already working for thousands.
Can I restart a statin after muscle pain went away?
Yes, if your symptoms have fully resolved for at least 2-4 weeks. Most people who stop statins due to muscle pain can restart safely with the right strategy-switching statins, lowering the dose, or using every-other-day dosing. The key is a structured plan, not just trying again randomly.
Which statin has the least muscle side effects?
Pravastatin and fluvastatin are the least likely to cause muscle pain. They’re cleared by the liver differently and don’t build up in muscle tissue like simvastatin or atorvastatin. Studies show switching to one of these is the most common reason people successfully restart statins.
Is muscle pain always from the statin?
No. In clinical trials, about 5% of people taking a placebo reported muscle pain-same as those on statins. Aging, low thyroid, vitamin D deficiency, or even inactivity can cause similar symptoms. The SAMS-CI tool helps separate true statin reactions from other causes.
What if I had rhabdomyolysis?
Do not restart any statin. Rhabdomyolysis is a serious condition where muscle breaks down dangerously. The American Heart Association advises permanent discontinuation. Talk to your doctor about alternatives like PCSK9 inhibitors or bempedoic acid.
How long should I wait before trying a statin again?
Wait 2-4 weeks after all muscle symptoms have completely disappeared. Waiting longer increases your heart risk without improving safety. Studies show muscle symptoms improve within this window after stopping the statin.
Can I use ezetimibe instead of a statin?
Ezetimibe alone lowers LDL by only 15-20%, which may not be enough for high-risk patients. It’s best used with a low-dose statin. If you can’t tolerate any statin, it’s a good standalone option, but not as effective as statins for preventing heart events.
Are PCSK9 inhibitors worth the cost?
For people who truly can’t take statins and have high cardiovascular risk (like prior heart attack or diabetes), yes. They reduce heart events by 15-17%. But they cost $5,850 a month. Insurance usually requires proof of statin intolerance before covering them. Rechallenge is cheaper and often just as effective.
Final Thought
You weren’t meant to live without statins. The data is clear: most muscle pain isn’t the statin’s fault. And when it is, there’s a way back. You don’t have to choose between heart health and muscle comfort. You can have both-if you know how to try again.
Scott Conner
February 7, 2026 AT 06:45so i stopped statins after my quads started feeling like wet sand after a 10k. thought i was done for. then i read this and tried pravastatin 10mg every other day. no pain. ldl still under 100. like… i didn’t even know this was a thing. why isn’t my doc telling me this?
Alex Ogle
February 7, 2026 AT 13:06look. i’m not some medical guru. i’m just a guy who’s been on statins for 12 years, had a mild case of myalgia, quit cold turkey, and then spent six months feeling like a ticking time bomb because my cardiologist said ‘just stay off it.’ then i found this protocol. 62% success rate? that’s not a fluke. that’s a systemic failure in primary care. doctors are scared to restart. patients are scared to ask. we’re all just floating in this limbo of misinformation. it’s not rocket science. it’s basic pharmacology. why are we making this so damn hard?
Tasha Lake
February 7, 2026 AT 23:14the SAMS-CI tool is a game-changer. i used it on myself after my doc dismissed my concerns. scored a 3. 91% chance of tolerance? i restarted on fluvastatin 10mg with psyllium husk and ezetimibe. 3 weeks later, CK was normal, symptoms gone. this isn’t anecdotal-it’s clinical. why isn’t this in every primary care office? it’s like we’re still using horse-drawn ambulances in 2024.
Andy Cortez
February 9, 2026 AT 13:34lol statins are just big pharma’s way of making you pay for their bad science. they know 5% of placebo users get muscle pain too. so why are we blaming the pill? maybe it’s your couch. maybe it’s your coffee. maybe it’s your fear. the nocebo effect is real, bro. you’re not sick. you’re just scared. stop taking the pill. start taking responsibility. also, i heard statins cause dementia. just saying.
Jacob den Hollander
February 9, 2026 AT 22:36i just want to say… thank you. really. i’ve been terrified to even think about statins again since my last episode. i thought i’d be off them forever. but reading this? it felt like someone handed me a map after i’d been wandering in the dark. i’m gonna ask my doc for the SAMS-CI test next week. and i’m switching to pravastatin. if it works? i’ll be back here to say thanks. you saved me from giving up on my heart.
Andrew Jackson
February 11, 2026 AT 12:55It is a profound failure of Western medicine that we have reduced the human body to a biochemical equation. Statins are not a panacea. They are a chemical intrusion into the natural order of human physiology. The body, when given rest, proper nutrition, and spiritual alignment, can regulate its own cholesterol. To suggest that one must rechallenge with a synthetic compound is to embrace a technocratic tyranny. I do not trust pharmaceutical protocols. I trust ancestral wisdom. And ancestral wisdom did not include statins.
PAUL MCQUEEN
February 13, 2026 AT 02:0660-80% success rate? really? where’s the peer-reviewed meta-analysis on that? i’ve seen studies with smaller n’s than this get shredded. also, who the hell is running these lipid clinics? are they just pulling numbers out of their ass? and why does every single statin have a different name? like, why can’t we just have one good one? this whole thing feels like a marketing scheme disguised as science.
Kathryn Lenn
February 14, 2026 AT 03:17so… the government and big pharma are secretly using statins to make us weak so we don’t protest? the muscle pain? it’s not side effects. it’s a control mechanism. and now they want us to ‘rechallenge’? like, no. i’m not falling for that. i’ve read about this before. they’re just trying to get us back on the drug so they can keep raking in billions. i’m taking turmeric and yoga. and i’m not alone.
Angie Datuin
February 16, 2026 AT 01:36i had the same thing. stopped simvastatin, felt better. then i started having chest tightness. turned out it wasn’t the statin. it was anxiety. but i didn’t know that until i did the whole MEDS thing. just… don’t assume. test. ask. you’re not crazy for feeling it. but you might be wrong about why.
Camille Hall
February 16, 2026 AT 15:11for anyone who’s been told ‘just live without statins’ - you’re not alone. i’ve been there. but this post? it gave me hope. i’m going to ask for the SAMS-CI. i’m switching to pravastatin. and i’m adding psyllium. if it works, i’ll post an update. if it doesn’t? i’ll still be glad i tried. because trying matters.
Ritteka Goyal
February 17, 2026 AT 17:12in india we dont have this problem because we eat more turmeric and garlic and dont sit all day like americans. also our doctors dont push statins like candy. i think its because you guys are too lazy and eat too much cheese. try yoga and walking 10k steps daily. then you dont need statins. i tried this and my cholesterol dropped. no pills. just discipline. you should try. your body will thank you. i am from india and we know better.
Jonah Mann
February 18, 2026 AT 10:43just a heads-up: if you’re on simvastatin and you’re over 65? check your SLCO1B1 gene. i didn’t know this existed until i got my 23andme results. *5 variant? yeah. that’s why i got wrecked. switched to pravastatin, 10mg daily, no issues. also, don’t forget to get your vitamin d checked. mine was at 18. fixed that, and my aches vanished. this whole thing? it’s not magic. it’s just… details. pay attention to the details.