Schizophrenia: Understanding Antipsychotic Medications and Atypical Agents

When someone is diagnosed with schizophrenia, the conversation often turns quickly to medication. It’s not just about managing voices or paranoia-it’s about reclaiming daily life. Antipsychotic drugs are the backbone of treatment, but not all are the same. Some work better for certain people, while others come with side effects that can be harder to live with than the symptoms themselves. The truth is, picking the right antipsychotic isn’t a one-size-fits-all decision. It’s a balancing act between symptom control, side effects, and long-term health.
First-Generation vs. Second-Generation Antipsychotics
The two main classes of antipsychotics are first-generation (FGAs) and second-generation (SGAs), also called atypical antipsychotics. FGAs, like haloperidol and chlorpromazine, were developed in the 1950s. They work mainly by blocking dopamine D2 receptors in the brain. That helps reduce hallucinations and delusions, but it often comes at a cost: movement problems. About 30 to 50% of people on these drugs develop stiffness, tremors, or restlessness-side effects known as extrapyramidal symptoms. These can be so uncomfortable that many stop taking the medication. SGAs came along in the 1980s and changed the game. Drugs like risperidone, olanzapine, quetiapine, and aripiprazole don’t just block dopamine. They also affect serotonin receptors, especially 5-HT2A. This dual action means they’re less likely to cause movement issues. They’re now the first-line choice for most people starting treatment, according to the American Psychiatric Association. But they’re not without problems. Some cause weight gain, high blood sugar, or high cholesterol. Olanzapine, for example, can lead to an average weight gain of 4.2 kilograms over a year. Aripiprazole and ziprasidone, on the other hand, are much gentler on the waistline.Which Antipsychotic Works Best?
There’s a myth that all antipsychotics are equally effective. That’s not true. A 10-year study of over 17,000 patients found clozapine had the longest time before people stopped taking it-over 500 days on average. Aripiprazole came in second, followed by paliperidone and olanzapine. Haloperidol, a first-gen drug, had the shortest duration: just 134 days. In another study of nearly 28,500 patients, those on aripiprazole had an 18.2% chance of relapse within a year. Those on haloperidol? Nearly 30%. Clozapine is the most effective for treatment-resistant schizophrenia-cases where two or more other drugs failed. But it’s not used first because of a rare but serious risk: agranulocytosis, a drop in white blood cells that can leave the body vulnerable to infection. The risk is 1-3%, which is why patients on clozapine need weekly blood tests for the first six months. Still, for those who respond, it can be life-changing. One patient on Reddit said, “After five failed medications, clozapine gave me my life back despite the blood tests.”Side Effects: The Hidden Trade-Offs
Choosing an antipsychotic often means choosing which side effects you can live with. Weight gain is a big one. Clozapine and olanzapine are the worst offenders, with average gains of 4.5kg and 4.2kg respectively. Quetiapine adds about 2.8kg. But aripiprazole and ziprasidone? Just 0.6kg on average. That’s a huge difference when you’re trying to avoid diabetes or heart disease. Movement problems flip the script. The drugs that cause the least weight gain-like risperidone and paliperidone-are more likely to cause stiffness or akathisia (that unbearable inner restlessness). About 18% of people on risperidone report movement issues. Aripiprazole has a lower rate at 4.1%, but 40% of new users on Reddit say akathisia made them want to quit. Clozapine, surprisingly, has the lowest movement disorder risk at just 1.8%. Sedation is another factor. Olanzapine and quetiapine make people very sleepy. That can help with insomnia or agitation, but it’s hard to function if you’re drowsy all day. Aripiprazole and lurasidone are less sedating, which makes them better for people who work or go to school.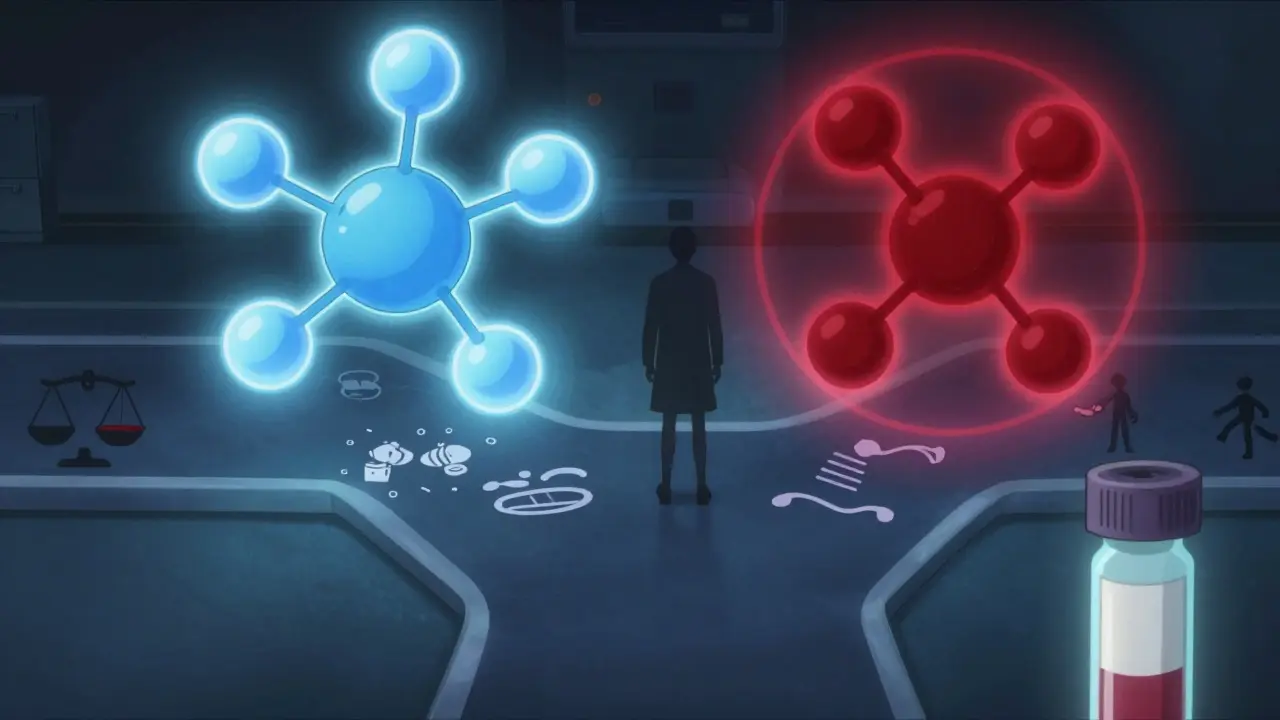
Long-Acting Injections and Real-World Adherence
Taking a pill every day sounds simple-until you’re feeling better and think you don’t need it anymore. Studies show that 63% of people stop their first antipsychotic within six months. That’s why long-acting injectables (LAIs) are becoming more common. These shots last weeks or months, so you don’t have to remember daily pills. Paliperidone palmitate, given once a month, cuts relapse rates by 22% compared to oral risperidone. In Europe, 30% of antipsychotic prescriptions are LAIs. In the U.S., it’s 25%. That gap isn’t just about preference-it’s about access, cost, and provider comfort. LAIs aren’t perfect. They can cause pain at the injection site, and once it’s given, you can’t take it back if side effects appear. But for people who’ve struggled with adherence, they’re a game-changer.What About New Drugs on the Horizon?
The field isn’t standing still. In 2023, the FDA approved lumateperone (Caplyta) for schizophrenia, with minimal weight gain and no movement side effects. Two drugs in late-stage trials show real promise: KarXT (xanomeline-trospium), which works through a completely different brain pathway, and SEP-363856, a TAAR1 agonist that reduces symptoms without causing weight gain. Even olanzapine is getting an upgrade: ALKS 3831 combines it with samidorphan to block the weight gain that usually comes with it. But here’s the catch: none of these new drugs have proven better than clozapine for treatment-resistant cases. And they’re expensive. Most are still brand-name, costing hundreds per month. Generic versions of older SGAs like aripiprazole can cost as little as $4 a month.Personalizing Treatment: It’s Not One Size Fits All
There’s no single “best” antipsychotic. The right one depends on your symptoms, your body, your lifestyle, and your goals. A young student might pick aripiprazole for its clear-headedness and low weight gain. Someone with severe insomnia and agitation might benefit from quetiapine’s sedating effect. A person with a history of diabetes might avoid olanzapine entirely. Doctors now use tools like pharmacogenetic testing to see how your body metabolizes drugs. People with certain gene variants (like CYP2D6 or CYP1A2) process medications differently. Testing can reduce side effects by 37%, according to a 2022 study. It’s not standard everywhere yet, but it’s becoming more common.
What to Expect When Starting
Starting an antipsychotic isn’t instant. It takes 2 to 4 weeks just to see if symptoms begin to shift. Dose adjustments happen slowly-often over 4 to 8 weeks. Too fast, and you risk akathisia or sedation. Too slow, and you might lose hope before it works. Monitoring is key. For clozapine, weekly blood tests for six months are mandatory. For others, a baseline metabolic panel (blood sugar, cholesterol, weight) is all you need. If you’re on a drug like olanzapine or quetiapine, your doctor should check your weight and blood sugar every 3 months.When Medication Isn’t Enough
Medication helps, but it’s not the whole picture. People who combine antipsychotics with therapy, social support, and structured routines do better long-term. Digital tools-apps that track symptoms, remind you to take pills, or connect you to peer groups-can reduce symptoms by 25% when used alongside meds. For the 30% of people who don’t respond to clozapine, options are limited. Some turn to electroconvulsive therapy (ECT), which has helped in cases where drugs failed. Others explore experimental treatments through clinical trials.Final Thoughts: Hope, Not Just Pills
Schizophrenia treatment has come a long way since chlorpromazine was first used in 1952. We now have tools to tailor treatment, reduce side effects, and improve quality of life. But progress isn’t just about new drugs-it’s about listening to patients. The person who says, “I can’t take the weight gain,” or “I can’t sleep through the day,” isn’t being difficult. They’re telling you what matters. The goal isn’t just to silence the voices. It’s to help someone live a full life-work, connect, grow. And that means choosing the right medication, not just the most popular one.Are atypical antipsychotics better than typical ones?
Yes, for most people. Atypical antipsychotics (second-generation) cause fewer movement disorders like tremors and stiffness, which are common with older drugs like haloperidol. They’re also more effective at treating negative symptoms like social withdrawal and lack of motivation. However, they can cause weight gain and metabolic issues, so the choice depends on your health history and personal priorities.
Why is clozapine only used as a last resort?
Clozapine is the most effective antipsychotic for treatment-resistant schizophrenia, but it carries a risk of agranulocytosis-a dangerous drop in white blood cells that can lead to life-threatening infections. Because of this, patients must get weekly blood tests for the first six months, and regular monitoring after that. The requirement makes it harder to prescribe and use, so doctors only turn to it after two other antipsychotics have failed.
Which antipsychotic causes the least weight gain?
Aripiprazole and ziprasidone cause the least weight gain-about 0.6 kilograms on average over a year. In contrast, clozapine and olanzapine can cause over 4 kilograms of weight gain. If weight management is a concern, these two are often preferred, especially for younger patients or those with diabetes risk factors.
Can I stop taking antipsychotics if I feel better?
Stopping suddenly can lead to a return of symptoms, sometimes worse than before. Even if you feel fine, antipsychotics work to prevent relapse, not just treat active symptoms. Most experts recommend staying on them long-term, especially after a first episode. If you want to reduce or stop, talk to your doctor first-tapering slowly under supervision is the safest approach.
Do antipsychotics cure schizophrenia?
No, antipsychotics don’t cure schizophrenia. They manage symptoms-hallucinations, delusions, disorganized thinking-by balancing brain chemicals. For many, they make daily life possible. But recovery also involves therapy, social support, stable housing, and purposeful activity. Medication is one part of a much bigger picture.
What are long-acting injectables, and are they right for me?
Long-acting injectables (LAIs) are antipsychotic medications given as shots every few weeks or months instead of daily pills. They’re helpful if you’ve struggled to take medication regularly. Studies show LAIs reduce relapse and hospitalization rates. Paliperidone palmitate and risperidone LAI are common options. They’re not for everyone-some people dislike injections, and side effects can’t be reversed once given. But for those who’ve had relapses due to missed doses, LAIs can be life-changing.
How long does it take for antipsychotics to work?
You might notice some improvement in agitation or sleep within a few days, but full symptom control usually takes 4 to 8 weeks. It often takes 2 to 3 months to find the right dose and medication combination. Patience is key. If you don’t see progress after 6 to 8 weeks, talk to your doctor about adjusting the dose or trying a different drug.
Is there a risk of addiction with antipsychotics?
Antipsychotics are not addictive. You won’t get high from them, and you won’t crave them like you might with alcohol or opioids. However, your body can become physically dependent on them. Stopping suddenly can cause withdrawal symptoms like nausea, insomnia, or a return of psychotic symptoms. Always taper off under medical supervision.
Donna Fleetwood
February 1, 2026 AT 09:37Just wanted to say this post gave me hope. I’ve been on three different meds over five years and finally found a combo that lets me work part-time and hang out with my niece without feeling like a zombie. It’s not perfect, but it’s progress. Keep fighting, everyone.
Diana Dougan
February 2, 2026 AT 00:53lol so basically we’re just trading one set of side effects for another? cool. next they’ll tell us the pill makes you smarter. oh wait-nope, just less likely to scream at the toaster. thanks for the 20-page ad copy, doc.
Bobbi Van Riet
February 3, 2026 AT 03:21I’ve been a psychiatric nurse for 18 years and I can’t stress enough how much the ‘one-size-fits-all’ myth hurts people. I had a client on olanzapine who gained 60 pounds in 9 months and quit because she couldn’t walk to her mailbox. Switched her to aripiprazole-lost 30 pounds in 6 months, started painting again. It’s not magic, it’s matching the drug to the person. Also, LAIs saved two of my patients from repeated hospitalizations. If your doc won’t bring it up, ask. Seriously.
Holly Robin
February 4, 2026 AT 11:15EVERYTHING YOU’RE TOLD ABOUT ANTIPSYCHOTICS IS A LIE. Big Pharma owns the APA, the FDA, and your doctor’s continuing ed. They push these drugs because they’re profitable-not because they’re safe. Aripiprazole? It’s a dopamine partial agonist-meaning it tricks your brain into thinking it’s balanced while slowly destroying your metabolism. And clozapine? They only use it as a last resort because it WORKS TOO WELL. They don’t want you cured. They want you dependent. Wake up.
Gaurav Meena
February 4, 2026 AT 13:53Great breakdown! As someone from India, I’ve seen how stigma makes people avoid meds entirely. But when families understand that this isn’t ‘weakness’-it’s biology-things change. My cousin started on quetiapine, struggled with sleepiness, switched to lurasidone, and now teaches yoga. Medication + community = real healing. 🙏
Katie and Nathan Milburn
February 6, 2026 AT 00:58The empirical data presented here is methodologically sound and aligns with current clinical guidelines as outlined in the 2020 APA Practice Guideline for the Treatment of Patients With Schizophrenia. The distinction between pharmacodynamic profiles and metabolic liabilities is well-articulated and merits clinical consideration.
kate jones
February 7, 2026 AT 20:51Pharmacogenomics is the future. CYP2D6 poor metabolizers on risperidone? They’re getting toxic levels. Ultra-rapid metabolizers on aripiprazole? No effect. Testing isn’t optional anymore-it’s standard of care. If your provider hasn’t mentioned it, ask for a pharmacogenetic panel. It’s covered by most insurers now. This isn’t sci-fi. It’s science.
Natasha Plebani
February 8, 2026 AT 00:09It’s funny how we treat schizophrenia like a broken circuit that needs a voltage fix. But what if the brain isn’t malfunctioning-it’s adapting? The voices, the paranoia-they’re responses to trauma, isolation, systemic neglect. Medication quiets the noise, sure. But what if the real treatment is rebuilding the world that broke the person in the first place? I’m not saying ditch the pills. I’m saying: don’t confuse suppression with healing.
Eliana Botelho
February 8, 2026 AT 21:56Wait, so you’re telling me the drug that works best-clozapine-is the one that makes you get blood drawn every week? That’s insane. Why not just give everyone a daily pill and let them die? Oh wait, that’s what we already do with the uninsured. And now you’re acting like this is some noble medical breakthrough? Newsflash: if you’re poor, you can’t afford the monitoring. If you’re homeless, you can’t keep up with the appointments. So yeah, ‘personalized treatment’ sounds great on paper-until you’re the one who can’t afford the paper.
Rob Webber
February 9, 2026 AT 01:54Everyone here is acting like antipsychotics are some miracle cure. They’re not. They’re chemical straitjackets. I was on olanzapine for two years. I gained 70 pounds. I couldn’t think clearly. I lost my job. My girlfriend left. And for what? So I could sit on the couch and not hear voices? I’d rather hear the voices than be a walking corpse. This system is broken and you’re all just drinking the Kool-Aid.
Lisa McCluskey
February 10, 2026 AT 12:55LAIs work. I’ve seen it. My brother went from 4 hospitalizations a year to zero after switching to paliperidone monthly. He still takes his pills when he’s stable. But knowing the shot’s coming keeps him grounded. It’s not about control. It’s about consistency.
Darren Gormley
February 11, 2026 AT 20:01😂😂😂 so aripiprazole is the ‘good’ one because it doesn’t make you fat? But it makes you feel like you’re being chased by bees inside your skull? That’s a win? And clozapine? Oh yeah, the one that kills your white blood cells-totally worth it if you’re rich enough to get weekly blood draws. Meanwhile, I’m on Medicaid and they won’t even approve the test. So I guess I’ll just die quietly. 😎
Mike Rose
February 13, 2026 AT 16:09all these meds are just brain drugs. why not just try yoga? or meditation? or eating less sugar? i heard someone cured their schizophrenia with kale. just saying.