Sepsis: Recognizing Early Warning Signs and Understanding Hospital Treatments
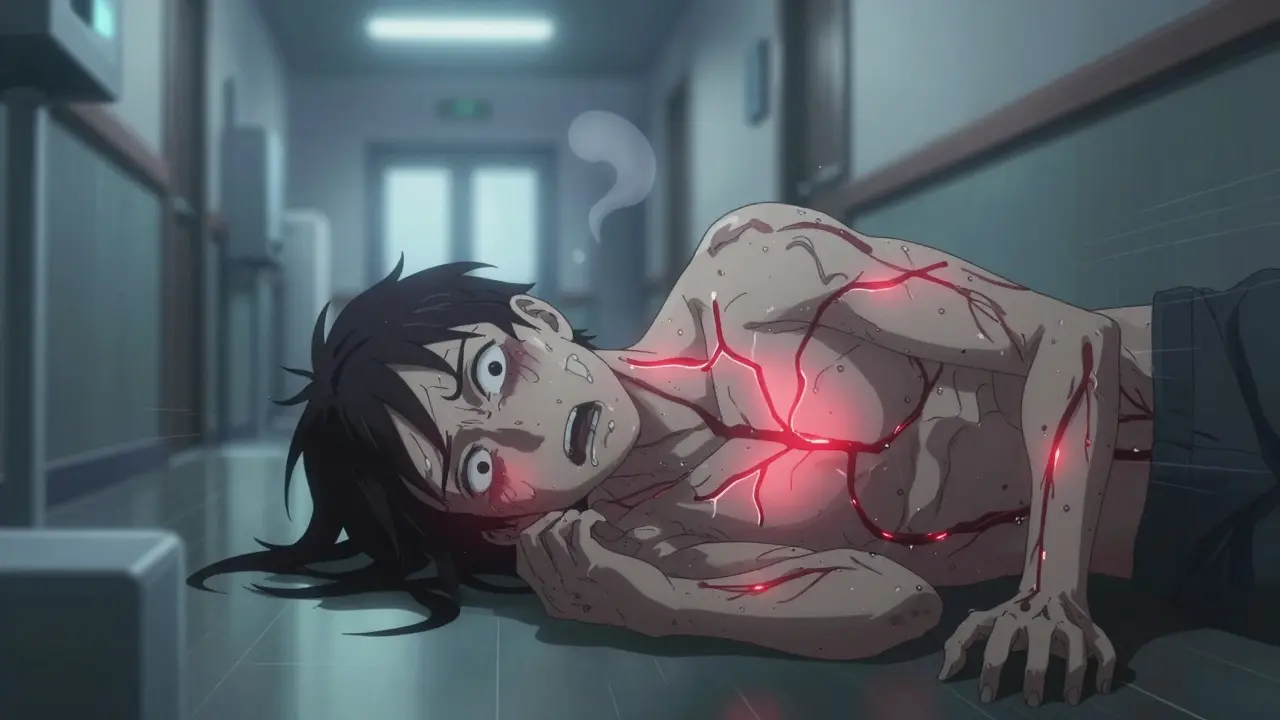
When you feel like you're dying and can't explain why, it might not be just the flu. Sepsis doesn't always start with a high fever or a cough. Sometimes, it starts with a quiet confusion, a strange paleness, or the overwhelming sense that something is terribly wrong - even if you can't point to exactly what. This isn't paranoia. It's your body screaming for help. Every year, sepsis kills more people than heart attacks, breast cancer, and prostate cancer combined. And the worst part? Many of those deaths happen because the signs are missed - by patients, by families, and sometimes even by doctors who don't act fast enough.
What Sepsis Really Is (And Why It's Not Just an Infection)
Sepsis isn't the infection itself. It's what happens when your body's immune system goes into overdrive trying to fight off an infection - and ends up attacking your own organs. This can happen from a simple urinary tract infection, a cut that got infected, pneumonia, or even after surgery. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), published in 2016, made this clear: sepsis is organ dysfunction caused by a dysregulated response to infection. That means your kidneys, lungs, liver, or heart start failing because your body is in chaos. This isn't a slow process. It can go from mild to life-threatening in hours. The key is catching it early. Studies show that if treatment starts within the first hour - what doctors call the "golden hour" - survival rates jump by up to 79%. That’s not a small difference. That’s the difference between going home and not coming home at all.The Six Signs You Can't Ignore
You don’t need a medical degree to spot sepsis. There are clear, urgent signs that should trigger an immediate trip to the ER. The Sepsis Alliance’s "TIME" mnemonic helps, but the real warning signs go deeper.- Temperature too high or too low: Over 38°C (100.4°F) or under 36°C (96.8°F). Fever isn’t always there - sometimes you’re cold and shivering, even under blankets.
- Infection signs: A wound that’s red, swollen, oozing; a cough that won’t quit; burning when you pee; or even just a recent surgery or hospital stay.
- Mental decline: Confusion, slurred speech, or being hard to wake up. In older adults, this is often the first and only sign. A 2019 study found 45% of sepsis patients had noticeable confusion before anything else.
- Extreme illness: The phrase "I feel like I might die" isn’t dramatic exaggeration - 78% of patients report saying this exact thing. It’s not anxiety. It’s your body’s alarm system going off.
- Slurred speech or confusion - happens in nearly half of cases.
- Extreme pain or discomfort - 67% of patients say it’s the worst pain they’ve ever felt, worse than childbirth or a broken bone.
- Pale, bluish, or blotchy skin - especially around lips, fingers, or toes. In children, this can look like mottled skin that doesn’t fade when you press on it.
- Sleepiness or trouble waking up - 52% of adults experience this. It’s not just tiredness. It’s a deep, unresponsive lethargy.
- Shortness of breath - breathing faster than 22 times per minute is a red flag. Your body is struggling to get oxygen because your organs are shutting down.
What Happens When You Get to the Hospital
If you or someone you love is showing these signs, don’t wait. Don’t call your doctor. Don’t try to "wait it out." Go to the ER. The moment you walk in, tell them: "I think I have sepsis." That phrase alone can speed things up dramatically. Hospitals follow strict protocols based on the Surviving Sepsis Campaign guidelines updated in 2021. The goal? Start treatment within one hour. This is called the "1-hour sepsis bundle." Here’s what happens:- Broad-spectrum antibiotics - given through an IV right away. Common choices are piperacillin-tazobactam or meropenem. These fight a wide range of bacteria while they figure out the exact cause.
- Blood cultures - taken before antibiotics, ideally within 30 minutes. This helps doctors later narrow down the infection source. Missing this step cuts survival chances by 18%.
- IV fluids - at least 30 mL per kilogram of body weight given within three hours. This helps stabilize blood pressure and keeps organs working.
- Serum lactate test - if levels are above 4 mmol/L, mortality risk jumps 40%. This tells doctors how badly your body is struggling.
- Oxygen therapy - if oxygen levels drop below 94%, you’ll get supplemental oxygen. Target is 94-98%.
- Urine output monitoring - doctors check how much you’re peeing. Less than 0.5 mL per kg per hour means your kidneys are failing.

What Happens After the Emergency
Getting past the first 24 hours doesn’t mean you’re out of danger. The next critical steps happen in the ICU.- Source control - doctors need to find and remove the infection’s origin. That could mean draining an abscess, removing a catheter, or even surgery.
- Glucose control - keeping blood sugar between 140-180 mg/dL. Too high or too low can make organ damage worse.
- Corticosteroids - hydrocortisone is given to patients who still need high doses of vasopressors. It doesn’t save lives outright, but it shortens shock by about a day and reduces ICU time.
- Targeted antibiotics - thanks to new tools like the Accelerate PhenoTest BC Kit (approved by the FDA in 2023), labs can identify bacteria and their resistance patterns in just 1.5 hours instead of days. That means better, faster antibiotics.
What Life Is Like After Sepsis
Surviving sepsis doesn’t mean returning to normal. A 2020 study of 1,500 survivors found that 60% still had crippling fatigue six months later. 45% couldn’t walk up stairs without gasping. 38% had constant body aches. 32% struggled with walking or balance. 29% couldn’t sleep properly. This is called post-sepsis syndrome. It’s real. It’s long-lasting. And it’s often ignored. The Cleveland Clinic found that 25% of survivors are readmitted within 30 days - mostly for new infections, breathing problems, or heart issues. Early rehab helps. Starting physical therapy within 72 hours of ICU admission reduces long-term disability by 22%. That’s why hospitals are now pushing for rehab teams to be part of the sepsis response from day one. And then there’s the cost. In the U.S., the average hospital stay for sepsis runs $18,000. Add ongoing care, rehab, and follow-ups, and it’s another $7,200 per year for survivors. That’s not just money - it’s time, energy, and quality of life.
Why Time Is Everything
Dr. Craig Coopersmith, president of the Society of Critical Care Medicine, says sepsis is like a stroke or heart attack: every hour without antibiotics increases death risk by 7.6%. That’s not a guess. That’s data. Hospitals with automated sepsis alert systems - triggered by vital signs like high heart rate, low blood pressure, or high lactate - cut time to antibiotics by 58 minutes on average. That’s enough to save 5.3% more lives. But here’s the ugly truth: Black patients in U.S. hospitals wait 18% longer for antibiotics and have 23% higher death rates than white patients. That’s not about individual doctors. It’s about systemic delays - from triage to testing to treatment. Awareness has improved since 2010, when only 19% of Americans could name even one sepsis symptom. By 2019, that number rose to 57%. But only 39% could name three. That’s why education matters - not just for patients, but for families, nurses, and first responders.What You Can Do
You don’t need to be a doctor to save a life. Here’s what you can do:- If someone feels like they might die - believe them.
- If they’re confused, pale, or breathing fast - don’t wait. Go to the ER.
- Speak up: "I think this is sepsis." That phrase gets attention.
- Know the signs for babies: no wet diaper, extreme sleepiness, fever.
- After recovery, push for rehab. Fatigue isn’t normal. It’s a symptom.
Can sepsis be treated at home?
No. Sepsis is a medical emergency that requires hospital care. Antibiotics must be given intravenously, fluids need precise monitoring, and vital signs must be tracked continuously. Trying to treat sepsis at home delays life-saving care and increases the risk of death.
Is sepsis contagious?
No, sepsis itself is not contagious. But the infection that triggers it - like pneumonia, a UTI, or a skin infection - can be. You can’t catch sepsis from someone else, but you can catch the bacteria or virus that might lead to it if your immune system is weakened.
How quickly does sepsis develop?
Sepsis can develop in hours. Someone might feel fine in the morning, have a fever by afternoon, and be in shock by night. That’s why early signs - like confusion, extreme pain, or shortness of breath - must never be ignored. The faster treatment starts, the better the chance of survival.
Can sepsis come back after treatment?
Yes. About one in four sepsis survivors are readmitted within 30 days, often because the infection wasn’t fully cleared or the immune system is still weakened. This is why follow-up care, including blood tests and monitoring for new infections, is critical after discharge.
Are there new treatments for sepsis?
Yes. In 2023, the FDA approved the Accelerate PhenoTest BC Kit, which identifies bacteria and antibiotic resistance in 1.5 hours instead of 2-3 days. This allows doctors to switch from broad-spectrum to targeted antibiotics faster. Research is also ongoing into immunomodulatory drugs like interferon gamma, which showed promise in reducing organ failure in early trials.
Why do some people survive sepsis and others don’t?
It’s not luck. Survival depends on three things: how fast treatment starts, the patient’s age and health before sepsis, and whether the infection source is removed quickly. Older adults, people with diabetes, cancer, or weakened immune systems are at higher risk. But even healthy people can die if treatment is delayed. Time is the biggest factor.
laura Drever
January 14, 2026 AT 01:31jefferson fernandes
January 15, 2026 AT 12:21James Castner
January 16, 2026 AT 02:02lucy cooke
January 16, 2026 AT 22:43Clay .Haeber
January 18, 2026 AT 12:06Priyanka Kumari
January 19, 2026 AT 20:06Vinaypriy Wane
January 20, 2026 AT 11:10Diana Campos Ortiz
January 20, 2026 AT 22:42