SGLT2 Inhibitors and Yeast Infections: What You Need to Know About Urinary Complications
SGLT2 Inhibitor Risk Calculator
Risk Assessment Tool
This tool helps you understand your personal risk of urinary complications while taking SGLT2 inhibitors based on clinical factors. According to recent studies, having 3 or more risk factors increases your chance of serious infection to over 15%.
When you’re managing type 2 diabetes, finding a medication that lowers blood sugar without causing low blood sugar or weight gain is a big win. That’s why SGLT2 inhibitors became so popular. Drugs like canagliflozin, dapagliflozin, and empagliflozin work in a clever way: they make your kidneys flush out extra sugar through urine. But here’s the catch - that same sugar doesn’t just disappear. It stays in your urinary tract, turning it into a breeding ground for yeast and bacteria.
How SGLT2 Inhibitors Work - and Why They Cause Infections
SGLT2 inhibitors block a protein in your kidneys that normally reabsorbs glucose back into your blood. Without that protein doing its job, up to 110 grams of sugar a day ends up in your urine. That’s the equivalent of about 22 teaspoons of sugar being flushed out daily. Sounds great for blood sugar control, right? But your body doesn’t just flush sugar - it flushes it into the area around your genitals and bladder. That’s where trouble starts.
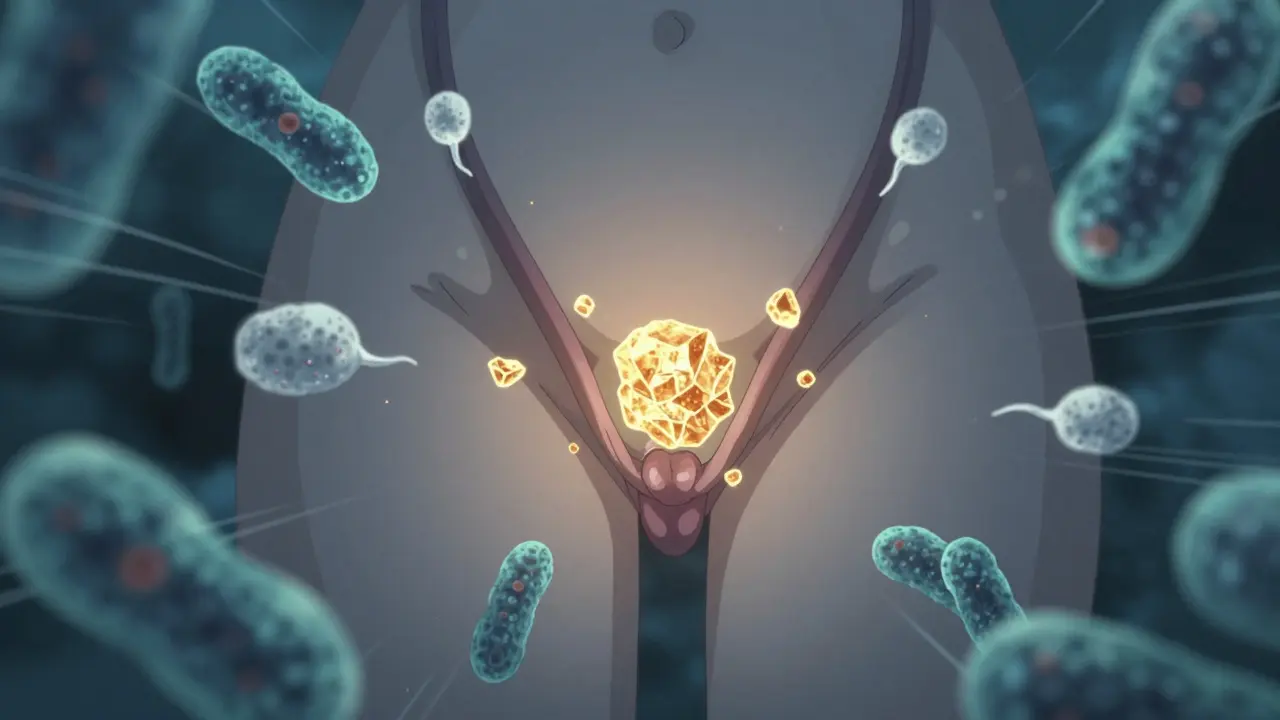
Yeast - especially Candida albicans - loves sugar. When glucose sits in your urine, it feeds the yeast already living in your genital area. For women, this often means recurring vulvovaginal candidiasis: itching, burning, thick white discharge. For men, it’s balanitis - redness, swelling, and pain under the foreskin. These aren’t just minor annoyances. In clinical trials, 3-5% of people taking SGLT2 inhibitors developed genital yeast infections, compared to just 1-2% on placebo. That’s a big jump.
It’s Not Just Yeast - Urinary Tract Infections Are a Real Risk
Yeast isn’t the only problem. Bacteria like Escherichia coli also thrive in sugary urine. The result? A higher chance of urinary tract infections (UTIs). Studies show people on SGLT2 inhibitors are nearly twice as likely to get a UTI compared to those on other diabetes drugs like DPP-4 inhibitors or sulfonylureas.
Most UTIs are mild - burning when you pee, needing to go often. But with SGLT2 inhibitors, they can turn serious fast. The FDA reviewed data from 2013 to 2014 and found 19 cases of urosepsis - a life-threatening bloodstream infection that starts in the urinary tract. All 19 required hospitalization. Four patients ended up in the ICU. Two needed dialysis because their kidneys failed. The average time from starting the drug to getting sick? Just 45 days.
When Things Get Dangerous: Complicated Infections
Some infections go beyond the bladder. One case report from the National Institutes of Health describes a 64-year-old woman who developed emphysematous pyelonephritis - a rare, gas-forming kidney infection that destroys tissue. She had no history of UTIs before starting dapagliflozin. After treatment, she felt better… until she restarted the drug 11 months later. The infection came back - worse than before. She needed surgery to drain an abscess around her kidney.
Even rarer, but deadly, is Fournier’s gangrene - a necrotizing infection that eats away at skin and tissue around the genitals and rectum. The European Medicines Agency added a warning about this in 2016. It’s rare - fewer than 1 in 10,000 users - but when it happens, it’s an emergency. Symptoms include severe pain, swelling, redness, fever, and a foul smell. If you notice any of these, go to the ER. Delaying treatment can cost you your life.

Who’s Most at Risk?
Not everyone on SGLT2 inhibitors gets infections. But some people are far more vulnerable:
- Women - due to shorter urethras and proximity of the genital tract to the anus
- People with a history of recurrent UTIs or yeast infections
- Those with poor genital hygiene
- People with diabetes complications like nerve damage (neuropathy), which can make it harder to feel early symptoms
- Older adults (over 65)
- People with kidney problems (eGFR below 60)
- Those with high HbA1c levels (above 8.5%) - more sugar in urine means more fuel for microbes
A 2024 study in Diabetes Care created a simple 5-point risk score. If you have three or more of the factors above, your risk of a serious UTI jumps to over 15%. That’s not just a small chance - it’s a red flag.
What Doctors Should Do - and What You Should Ask
The American Diabetes Association says: Check for past urinary infections before prescribing SGLT2 inhibitors. If you’ve had three or more UTIs in the last year, your doctor should consider other options - like GLP-1 agonists or DPP-4 inhibitors - which don’t carry this risk.
But if you’re already on an SGLT2 inhibitor and doing well for your heart and kidneys, don’t panic. These drugs reduce heart attacks, strokes, and kidney failure in high-risk patients. The benefits often outweigh the risks - if you’re monitored.
Ask your doctor:
- “Do I have a history that makes me more likely to get these infections?”
- “Should I be tested for yeast or bacteria before starting this drug?”
- “What symptoms should I report right away?”
And here’s what you can do yourself:
- Wipe front to back after using the bathroom
- Change out of wet clothes or swimsuits quickly
- Avoid scented soaps, douches, or bubble baths
- Drink plenty of water - at least 2 liters a day - to flush out sugar
- Consider cranberry supplements - a 2023 FDA review found they reduced UTIs by 29% in SGLT2 users, though they’re not FDA-approved for this use
What Happens If You Get an Infection?
If you develop symptoms - itching, burning, fever, pain, or unusual discharge - don’t wait. Don’t assume it’s “just a yeast infection.” Get checked. A simple urine test can tell if it’s yeast, bacteria, or something worse.
Treatment depends on the infection:
- Yeast: Over-the-counter antifungals (clotrimazole, miconazole) often work. If it keeps coming back, your doctor may prescribe oral fluconazole.
- Simple UTI: Antibiotics like nitrofurantoin or trimethoprim-sulfamethoxazole.
- Complicated UTI or kidney infection: IV antibiotics, hospital stay, sometimes surgery.
Here’s the hard truth: if you’ve had a serious infection while on an SGLT2 inhibitor, restarting the drug is risky. In the NIH case, the patient’s infection returned within months of restarting dapagliflozin. Many endocrinologists will avoid re-prescribing these drugs after a severe episode.
Are There Better Alternatives?
Yes - and they’re getting better.
GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and liraglutide (Victoza) lower blood sugar, help with weight loss, and protect the heart - without increasing yeast or UTI risk. They’re now recommended as first- or second-line options for people with heart disease or obesity.
DPP-4 inhibitors like sitagliptin and linagliptin have almost no infection risk. They’re weaker at lowering blood sugar than SGLT2 inhibitors, but they’re safe for people with recurrent UTIs.
Metformin remains the first choice for most people. It doesn’t cause weight gain or infections. But if you can’t take it - or if you need more help - newer options are available.
The Big Picture: Benefits vs. Risks
SGLT2 inhibitors are not bad drugs. They’ve changed how we treat diabetes. In the EMPA-REG trial, empagliflozin cut heart-related deaths by 38% in people with heart disease. In the DAPA-CKD trial, dapagliflozin slowed kidney failure in patients with chronic kidney disease - even if they didn’t have diabetes.
But these benefits come with a cost. The infection risk is real, predictable, and preventable. The key isn’t avoiding SGLT2 inhibitors entirely - it’s using them wisely.
For someone with heart failure and no history of infections? SGLT2 inhibitors might be the best choice.
For someone with three UTIs in the last year? Maybe not.
It’s not about the drug. It’s about the person.
What to Do Next
If you’re on an SGLT2 inhibitor:
- Know the warning signs - itching, burning, fever, swelling, pain
- Keep a log of any symptoms - even if they seem minor
- Don’t ignore a single episode of yeast - it could be a sign of a pattern
- Ask your doctor about your personal risk score
- Consider switching if infections keep coming back
If you’re thinking about starting one:
- Ask if your history makes you high-risk
- Compare it to alternatives - GLP-1s, DPP-4s, or even newer combo pills
- Understand that the benefit is strongest if you have heart disease, kidney disease, or obesity
- Don’t let the convenience of one pill outweigh the risk of a hospital stay
These drugs work. But they’re not magic. They’re tools. And like any tool, they’re safest when you know how they can hurt you - and how to stop it before it starts.
William Liu
December 20, 2025 AT 22:12SGLT2 inhibitors saved my life after my heart attack. I had zero infections because I drank water like it was my job and wiped front to back religiously. It’s not the drug’s fault - it’s about how you manage it.
mary lizardo
December 22, 2025 AT 03:28The assertion that cranberry supplements reduce UTIs in SGLT2 inhibitor users is scientifically unsubstantiated and misleading. The FDA review cited does not endorse this application, and conflating observational data with clinical recommendation constitutes a breach of medical communication ethics.
Erica Vest
December 23, 2025 AT 23:44For anyone on an SGLT2 inhibitor, I can’t stress enough: get a baseline urine culture before starting. If you’ve had recurrent yeast or UTIs, that’s your red flag. I’ve seen too many patients ignore early symptoms until they’re septic. Prevention isn’t optional - it’s non-negotiable.
Chris Davidson
December 25, 2025 AT 07:14People blame the drug but ignore hygiene. You pee sugar out your urethra and then sit in wet clothes? That’s not the medication’s problem. That’s your laziness. Wash up. Drink water. Stop making everything someone else’s fault
Kinnaird Lynsey
December 25, 2025 AT 15:50Wow. This post reads like a horror movie script. I’m just here wondering if I should be terrified or just… mildly concerned. I guess I’ll keep my pill and my cotton underwear.
benchidelle rivera
December 25, 2025 AT 20:34If you’re not actively monitoring for infections while on SGLT2 inhibitors, you’re not managing your diabetes - you’re gambling with your organs. This isn’t a ‘maybe’ risk. It’s a guaranteed consequence for anyone who ignores the signs. Your kidney isn’t a suggestion - it’s mandatory. Get tested. Stay informed. Or don’t. But don’t act surprised when you end up in the ICU.
Anna Sedervay
December 27, 2025 AT 06:40Have you ever considered that the pharmaceutical industry deliberately engineered these drugs to create recurring infections? Think about it - more infections mean more prescriptions, more hospital visits, more profit. The FDA is complicit. The medical establishment is asleep. They want you dependent. They want you afraid. And they want you buying more pills. Don’t be fooled.
Ashley Bliss
December 28, 2025 AT 22:21It’s not just about sugar in the urine - it’s about the soul’s surrender to modern medicine. We’ve traded presence for pills, awareness for convenience, and now we’re paying with our most intimate bodily sanctuaries. This isn’t a side effect - it’s a spiritual betrayal. We are no longer healing - we are outsourcing our vulnerability to a system that profits from our brokenness.
Mahammad Muradov
December 29, 2025 AT 04:37My cousin got Fournier’s gangrene on dapagliflozin. He was fine for six months. Then one day he couldn’t sit. No fever. No warning. Just pain. Then swelling. Then they cut half his groin off. He’s alive. But he’ll never walk the same. Don’t be like him. Ask your doctor if you’re worth the risk.