Statins and Antifungal Medications: How Their Interaction Raises Rhabdomyolysis Risk

Statins and Antifungals Interaction Checker
Check Your Medication Safety
Select your statin and antifungal to see if they can be safely combined. This tool helps you understand the risk of rhabdomyolysis and provides recommendations to stay safe.
When you take a statin to lower your cholesterol, you’re doing something smart for your heart. But if you also need an antifungal for a stubborn infection-like athlete’s foot, yeast infection, or ringworm-you could be putting yourself at serious risk. The problem isn’t the drugs themselves. It’s what happens when they meet inside your body. This isn’t a rare edge case. It’s a well-documented, preventable danger that sends people to the hospital every year.
Why This Interaction Is So Dangerous
Statins like simvastatin, lovastatin, and atorvastatin work by blocking an enzyme in your liver that makes cholesterol. But your body doesn’t just get rid of these drugs by passing them out. They’re broken down by a group of liver enzymes called CYP3A4. That’s where antifungals come in. Azole antifungals-like itraconazole, voriconazole, and even fluconazole-shut down CYP3A4 like flipping a switch. When that happens, your statin doesn’t get cleared. It builds up. And when it builds up too much, it starts tearing down your muscle tissue.This isn’t just muscle soreness. It’s rhabdomyolysis-a condition where muscle cells break apart and spill their contents into your bloodstream. That can clog your kidneys, cause kidney failure, and in severe cases, kill you. The numbers don’t lie: statins alone cause rhabdomyolysis in about 0.1 to 0.5 cases per 10,000 people each year. But when you add a strong antifungal like itraconazole? That risk jumps 10 to 20 times higher.
Which Statins Are Most at Risk?
Not all statins are created equal when it comes to this interaction. Your risk depends on how much your body relies on CYP3A4 to clear the drug.- High risk: Simvastatin, lovastatin, and atorvastatin. These are broken down almost entirely by CYP3A4. Take them with itraconazole, and simvastatin levels can spike by more than 1,000%. That’s why the FDA says you should never take simvastatin over 20 mg with itraconazole or ketoconazole.
- Moderate risk: Pitavastatin. It’s partially processed by CYP3A4. Studies show its levels can rise by about 2.5 times with voriconazole-but it’s less likely to cause severe muscle damage than simvastatin.
- Low risk: Pravastatin, fluvastatin, and rosuvastatin. These barely touch CYP3A4. They’re cleared through other pathways. That’s why doctors often switch patients to these when an antifungal is needed.
Here’s what that looks like in real numbers: A 2017 study found that taking itraconazole with simvastatin increased the active form of the drug in your blood by 10 times. With lovastatin? Up to 15 times. That’s not a typo. Fifteen times more drug than your body was designed to handle.
Which Antifungals Are the Worst Offenders?
Not all antifungals are equally dangerous. Their strength as CYP3A4 blockers varies widely.- Strong inhibitors: Ketoconazole, itraconazole, voriconazole. These are the biggest threats. The FDA explicitly warns against combining them with simvastatin and lovastatin. Even atorvastatin needs caution.
- Moderate inhibitor: Fluconazole. It’s weaker, but still dangerous-especially at high doses. A 400 mg daily dose of fluconazole can bump simvastatin levels by 350%. That’s why guidelines say if you must take fluconazole, your simvastatin dose should never go above 10 mg per day.
- Low risk: Isavuconazole. Approved in 2015, this newer antifungal barely touches CYP3A4. It’s becoming the go-to choice for patients on statins who need long-term antifungal therapy.
One 2023 study found that fluconazole and fluvastatin showed a surprising synergy against Candida albicans-meaning they worked better together against the fungus. But that doesn’t make it safe. The same combination still raises statin levels dangerously. Therapeutic synergy doesn’t cancel out toxicity.
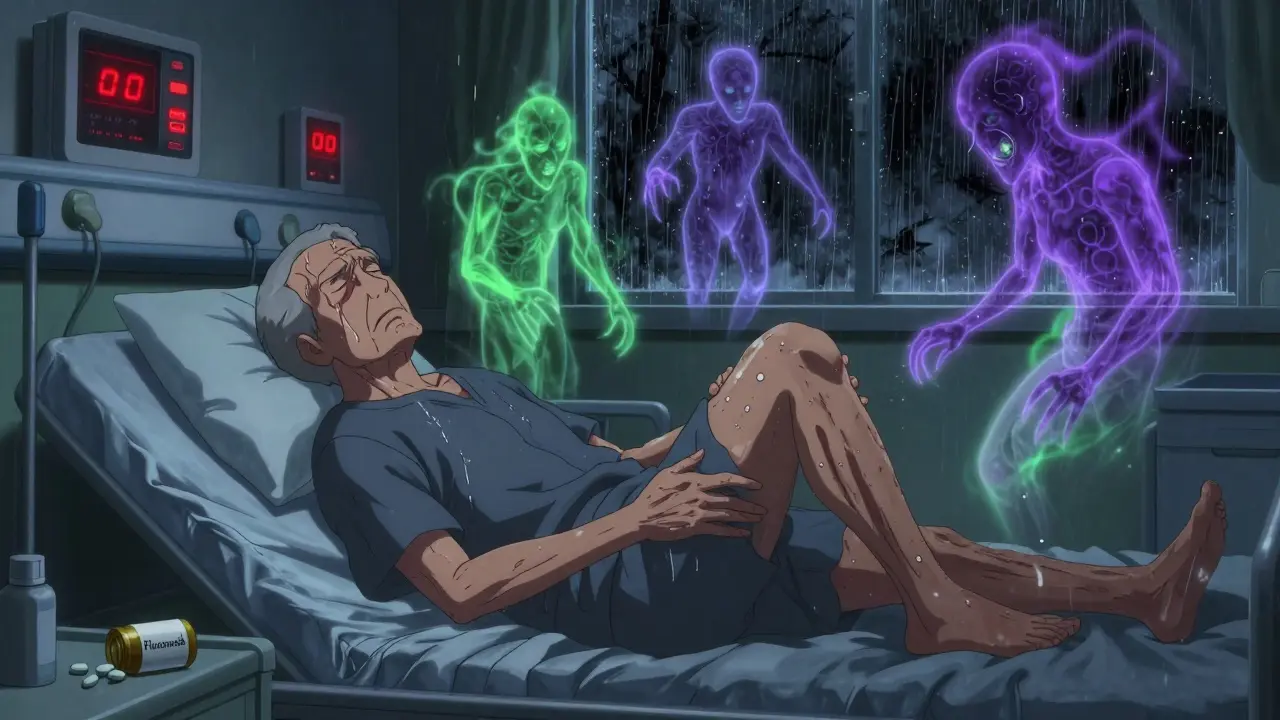
Real Cases, Real Consequences
This isn’t theoretical. People are getting sick because of this interaction.In 2018, a 68-year-old man in the U.S. was prescribed fluconazole 200 mg daily for toenail fungus. He was already taking simvastatin 40 mg. Seven days later, he was hospitalized with creatine kinase (CK) levels at 18,400 U/L. Normal is 30-200. He had rhabdomyolysis. He spent three days in the hospital.
Pharmacists on Reddit’s r/Pharmacy report seeing 2-3 cases per year-mostly older patients with multiple health problems who didn’t realize their yeast infection treatment was clashing with their heart medication. One case involved a woman on simvastatin who got a fluconazole prescription for vaginal candidiasis. She didn’t tell her pharmacist she was on a statin. Two weeks later, she couldn’t walk. Her CK was over 10,000.
A review of FDA reports from 2010 to 2019 found 1,247 cases of rhabdomyolysis tied to statin-azole combinations. The most common pairing? Simvastatin and itraconazole (38.7% of cases). Next? Simvastatin and fluconazole (29.4%).
Symptoms? Severe muscle pain (92% of cases), weakness (88%), and dark, tea-colored urine (76%). These don’t show up overnight. They creep in over 7 to 14 days. That’s why people ignore them-thinking it’s just soreness from the gym or the flu.
What Doctors Should Do
Good prescribing means knowing the risks before writing the script.- For strong antifungals (itraconazole, voriconazole, ketoconazole): Stop simvastatin and lovastatin completely. Switch to pravastatin, fluvastatin, or rosuvastatin during treatment. Restart the original statin 2-3 days after the antifungal ends.
- For fluconazole: If simvastatin is necessary, cap it at 10 mg/day. For atorvastatin, don’t exceed 20 mg/day. Rosuvastatin (20 mg) and pravastatin (40 mg) are safer alternatives.
- For new prescriptions: Always check for statin use before prescribing any azole antifungal. Don’t assume the patient knows about the risk.
Many hospitals now use electronic health record systems with hard stops. Epic, for example, blocks prescriptions for simvastatin over 20 mg if itraconazole is already on file. At Mayo Clinic, this cut dangerous combinations by 87%.

What You Should Do
If you’re on a statin and your doctor prescribes an antifungal, ask these questions:- Is this antifungal a CYP3A4 inhibitor? (Ask for the name-ketoconazole, itraconazole, voriconazole, or fluconazole?)
- Which statin am I on? Is it simvastatin, lovastatin, or atorvastatin?
- Do I need to stop my statin while I take this antifungal? If so, what’s the safe alternative?
- Should I get my creatine kinase checked before and during treatment?
- What symptoms should I watch for? If I feel sudden muscle pain or notice dark urine, what do I do?
If you’re taking simvastatin or lovastatin and get a fluconazole prescription for a yeast infection, don’t just refill it. Call your pharmacy or doctor. Ask if it’s safe. It’s not your job to know the science-but it is your job to ask.
The Bigger Picture
About 36 million Americans take statins. Millions more get antifungals every year. The overlap is huge. And despite warnings from the FDA since 2012, a 2022 study found nearly 1 in 5 patients still got a dangerous combination. The rate was even higher in older adults and in outpatient clinics.The economic cost? A single rhabdomyolysis hospitalization can run $15,000 to $50,000. But the human cost? That’s harder to measure. It’s the man who can’t walk to his car. The woman who can’t hold her grandchild. The family that loses someone because a simple question was never asked.
Thankfully, things are improving. Newer antifungals like isavuconazole are safer. Pharmacogenomics is starting to identify people who are genetically more vulnerable. And awareness is growing. Between 2015 and 2022, rhabdomyolysis cases from this interaction dropped by 34%-thanks to better systems, better education, and better communication.
You don’t need to be a doctor to protect yourself. You just need to ask. And if your doctor doesn’t know the answer? Get a second opinion. Your muscles-and your life-depend on it.
Can I take fluconazole with my statin?
It depends on which statin you’re taking. If you’re on simvastatin or lovastatin, fluconazole can still be dangerous-even though it’s weaker than itraconazole. The safest approach is to avoid fluconazole with those two. If you’re on atorvastatin, your dose should be capped at 20 mg daily. For pravastatin, fluvastatin, or rosuvastatin, fluconazole is generally safe at standard doses. Always check with your doctor or pharmacist before combining them.
What are the signs of rhabdomyolysis?
The most common signs are severe muscle pain, especially in the shoulders, thighs, or lower back; extreme weakness; and dark, tea-colored urine. Some people also feel nauseous, have a fever, or feel generally unwell. If you notice any of these after starting an antifungal, stop the medication and seek medical help immediately. Don’t wait. High creatine kinase levels can damage your kidneys fast.
Is there a statin that’s safe with all antifungals?
Yes. Pravastatin, fluvastatin, and rosuvastatin are the safest choices when you need an antifungal. They don’t rely heavily on the CYP3A4 enzyme, so they’re much less likely to build up to toxic levels. If you’re on simvastatin or lovastatin and need long-term antifungal treatment, ask your doctor about switching to one of these. It’s a simple change that can prevent a life-threatening reaction.
How long after stopping an antifungal can I restart my statin?
Wait 2 to 3 days after your last dose of the antifungal before restarting your statin. This gives your liver time to clear the antifungal and restore normal CYP3A4 function. Restarting too soon-even one day later-can still lead to dangerous drug buildup. Your doctor should give you a clear timeline. If they don’t, ask.
Why don’t more doctors know about this interaction?
Many doctors aren’t pharmacologists. They focus on treating infections or heart disease, not drug metabolism. Plus, fluconazole is so common for yeast infections that it’s often prescribed without checking for statin use. That’s why pharmacist-led reviews and EHR alerts are so important. If your doctor doesn’t mention the risk, it’s up to you to ask. You’re your own best advocate.

Paul Ong
January 1, 2026 AT 19:31Been on simvastatin for years and just got prescribed fluconazole for a yeast infection. I called my pharmacist before refilling-thank god I did. They flagged it immediately. Don't be that guy who ignores the warning. Your muscles will thank you.
Stay smart.
Andy Heinlein
January 3, 2026 AT 13:49bro i had this happen to my uncle-he was on simva and took fluconazole for athlete’s foot. ended up in the er with dark urine and couldnt walk for a week. doc said if he waited another day he mightve lost a kidney. dont be cool about this shit. ask questions.
also why do they even still prescribe simvastatin like its 2005?
gerard najera
January 3, 2026 AT 21:16Drugs are not neutral. They are forces in a system. CYP3A4 is a gatekeeper. Block it, and chaos follows.
Knowledge is the only buffer.
Stephen Gikuma
January 5, 2026 AT 09:20Big Pharma knows this. They let it happen. Why? Because hospital bills make them richer. They don’t care if you lose your legs. They care about your insurance card.
Fluconazole is a trap. It’s designed to keep you dependent. And your statin? That’s the leash.
Wake up.
They’re selling sickness, not health.
Bobby Collins
January 5, 2026 AT 14:15okay but like… why does this keep happening? i mean, i get it’s science but like… why is no one stopping it? why are doctors just signing papers without reading? i swear if i get a script for fluconazole and i’m on a statin i’m gonna scream at the front desk. i’m not dying because someone didn’t check a box.
also can we talk about how weird it is that we trust pills we don’t understand?
Layla Anna
January 6, 2026 AT 19:49My mom just got prescribed itraconazole for ringworm and she’s on rosuvastatin-thankfully safe! 😊 But I made her call her pharmacist before taking it. She was like ‘I didn’t think it mattered’…
Guys, this stuff is real. It’s not hype. I’ve seen people in pain from this. Please, please ask. Even if it feels dumb. Your body is worth it. 💛
Also, isavuconazole sounds like a superhero drug. More of that please!!
Heather Josey
January 7, 2026 AT 22:34This is precisely why interdisciplinary collaboration in healthcare is non-negotiable. Pharmacists are the unsung heroes here. Their alerts prevent catastrophic outcomes daily. Yet, many providers still treat them as order-takers rather than clinical partners.
Systemic change requires both technological safeguards-like EHR hard stops-and cultural shifts in provider education. We must institutionalize this awareness, not rely on patient advocacy alone.
Thank you for this comprehensive breakdown. It’s a model for patient safety communication.
Donna Peplinskie
January 9, 2026 AT 05:56I’ve been a pharmacist for 18 years, and I still get stunned when I see simvastatin + fluconazole on the same script. It’s like someone handed a loaded gun to a toddler and said, ‘Hope you remember to point it away.’
My advice? If you’re on a statin and need antifungals, ask for pravastatin or rosuvastatin. Always. No exceptions. And if your doctor says, ‘It’s fine,’ ask them to show you the guideline. If they can’t, find someone who can.
Don’t let your next muscle ache be your last walk.
Olukayode Oguntulu
January 10, 2026 AT 16:27Let us not conflate pharmacokinetic interference with systemic pathology. The CYP3A4 axis is but one node in a complex metabolic lattice-reductionist narratives obscure the epistemic hierarchy of drug interaction discourse. One must interrogate the ontological primacy of enzyme inhibition as a causal vector, rather than accept pharmaceutical hegemony’s simplistic binary: safe/unsafe.
Moreover, the commodification of metabolic vulnerability under neoliberal biomedicine renders the patient not as subject, but as data point in a pharmacoeconomic feedback loop.
Isavuconazole? A palliative solution. The disease is the system.
Dusty Weeks
January 10, 2026 AT 21:11just read this and i swear to god i was on simva and took fluconazole last year and didn’t think twice… i’m alive but my legs hurt for like 3 weeks. i thought it was just from hiking.
my bad. 😅
if you’re on statins and get a fungal script-stop. call. ask. don’t be me.
also i’m switching to rosuvastatin. no more drama.