Steroids and NSAIDs Together: Why This Combo Raises GI Bleeding Risk and How to Prevent It
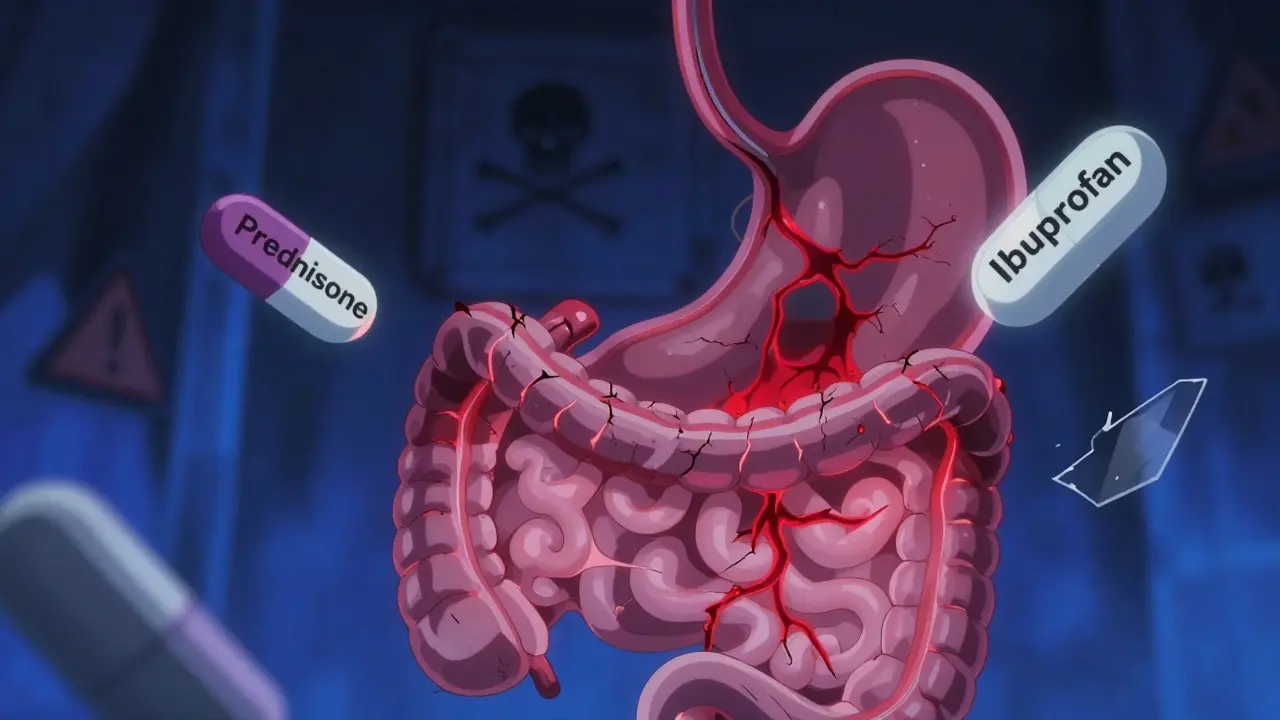
When you take a steroid like prednisone for inflammation and an NSAID like ibuprofen for pain, you might think you’re just managing two separate problems. But together, these drugs can quietly turn your digestive tract into a ticking time bomb. The risk isn’t small-it’s 12 times higher than taking either drug alone. And most people don’t even know it.
Why This Combination Is So Dangerous
NSAIDs work by blocking enzymes called COX-1 and COX-2. COX-2 helps with pain and swelling, but COX-1 is the body’s natural protector of the stomach lining. When NSAIDs shut down COX-1, they reduce the mucus and blood flow your stomach needs to stay healthy. That’s why some people get heartburn or ulcers after taking ibuprofen for weeks. Steroids make this worse. They don’t just cause irritation-they interfere with healing. If an ulcer starts forming, steroids slow down the repair process. They also dull the pain signals, so you might not notice the warning signs until it’s too late. Studies show that when you combine steroids with NSAIDs, the chance of a serious GI bleed jumps from about 1 in 1,000 to nearly 1 in 80 over a few months. And it’s not just stomach ulcers. About one-third of these bleeds happen lower down-in the small intestine or colon. These are harder to detect and often more deadly. One study found that 86% of people with lower GI bleeding had taken NSAIDs, even if they didn’t have a history of ulcers.Who’s at the Highest Risk?
Not everyone who takes both drugs will bleed. But certain people are in the danger zone:- People over 65
- Those with a past history of stomach ulcers or GI bleeding
- Anyone on blood thinners like warfarin or aspirin
- Patients on high-dose NSAIDs (ibuprofen over 1,200 mg/day, diclofenac over 100 mg/day)
- Anyone taking steroids for more than a week-even a short 5-day burst raises risk
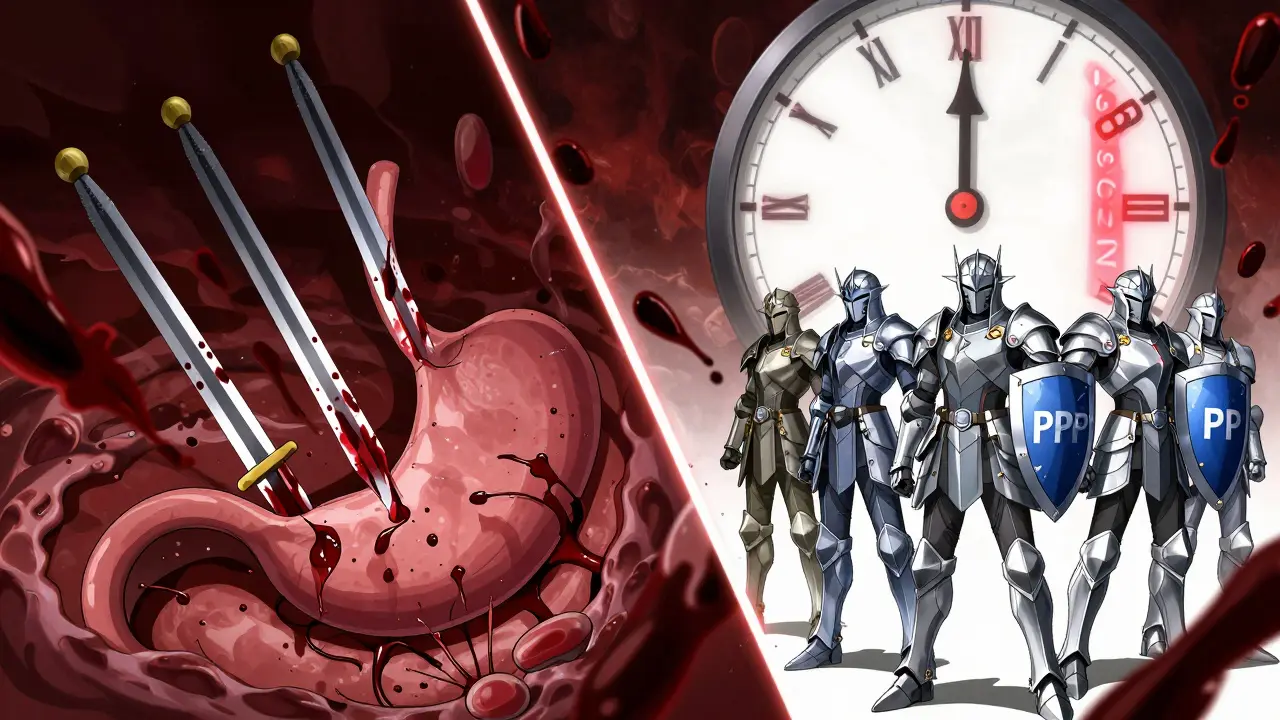
What Actually Works to Prevent Bleeding
The good news? This risk is almost entirely preventable. The gold standard is a proton pump inhibitor (PPI). Drugs like omeprazole, esomeprazole, or pantoprazole block acid production at its source, letting the stomach lining heal and stay protected. Studies show PPIs reduce NSAID-related ulcers by 73% compared to no protection. Here’s what the guidelines say:- Low-risk patients: One daily dose of omeprazole 20 mg (or equivalent) while taking both drugs.
- High-risk patients: Double the dose-omeprazole 40 mg daily-especially if you’ve had a prior bleed, are over 65, or take blood thinners.

Are Some NSAIDs Safer Than Others?
Yes. Traditional NSAIDs like naproxen and ibuprofen are the biggest culprits. But COX-2 inhibitors like celecoxib (Celebrex) were designed to spare the stomach. Studies show they cause 50-60% fewer ulcers than older NSAIDs. But here’s the catch: even celecoxib isn’t safe with steroids. The risk drops, but it doesn’t disappear. One trial showed that combining celecoxib with a PPI cut recurrent bleeding by 54% compared to naproxen with a PPI. Still, if you’re on steroids, your doctor should avoid naproxen or diclofenac altogether. There’s also a newer option: Vimovo, a single pill that combines naproxen with esomeprazole. It’s approved for high-risk patients and reduces ulcers by more than half compared to naproxen alone. But it’s expensive and not always covered by insurance.What Doctors Often Get Wrong
Many prescribers still think:- “It’s just a short steroid course-no need for protection.”
- “The patient’s fine-no stomach pain.”
- “I’ll just give them Tums or famotidine.”
What You Can Do Right Now
If you’re taking steroids and NSAIDs together:- Check your prescriptions. Are you on naproxen, ibuprofen, or diclofenac? If yes, ask your doctor if a PPI is needed.
- Don’t assume OTC NSAIDs are safe. Taking Advil daily and a steroid for allergies? That’s still risky.
- Ask if you can switch to celecoxib (if appropriate) or use Vimovo if available.
- Don’t stop the PPI just because your steroid course ends. Keep it going as long as you’re on NSAIDs.
- Know the warning signs: black or tarry stools, vomiting blood, sudden dizziness, or severe abdominal pain. Call your doctor immediately.
The Bigger Picture
This isn’t just about individual choices. It’s a system failure. In the U.S., over 21 million people get NSAIDs every year. Nearly 30% of them also get steroids. That’s millions of people walking around with a hidden risk. Health systems that use automated alerts-like Kaiser Permanente or Mayo Clinic-have cut bleeding events by over 68% by making PPIs automatic when both drugs are prescribed. Community clinics? Only 32% do it consistently. The cost of ignoring this? $1.87 billion a year in U.S. healthcare spending. And thousands of preventable hospitalizations. New research is looking at genetic testing to predict who’s most vulnerable to this combo. But until then, the solution is simple: if you’re on steroids and NSAIDs, you need a PPI. No debate. No exceptions.Frequently Asked Questions
Can I take ibuprofen with prednisone if I use antacids like Tums?
No. Antacids like Tums, Rolaids, or Maalox only neutralize acid temporarily. They don’t protect the stomach lining from NSAID damage or help ulcers heal. Only proton pump inhibitors (PPIs) like omeprazole or esomeprazole provide real protection. Using antacids instead of a PPI is like putting a bandage on a broken bone.
Is it safe to take a steroid for a few days with an NSAID if I have no stomach problems?
No. Even a 5- to 7-day steroid burst combined with NSAIDs can trigger a bleed. Many patients have no symptoms until they’re actively bleeding. Studies show the risk rises within days of starting both drugs. If you’re prescribed both, you should get a PPI-even if you feel fine.
Are COX-2 inhibitors like celecoxib safe with steroids?
They’re safer than traditional NSAIDs like naproxen, but not risk-free. Celecoxib cuts GI bleeding risk by about half compared to older NSAIDs. But when combined with steroids, the risk still rises significantly. Always pair celecoxib with a PPI if you’re on steroids. Never assume it’s safe without protection.
How long should I stay on a PPI if I’m on steroids and NSAIDs?
Stay on the PPI for as long as you’re taking the NSAID. The steroid course may end in a week or two, but if you’re still using ibuprofen or naproxen for arthritis or back pain, you still need protection. Stopping the PPI too early is a common mistake that leads to preventable bleeds.
What if I can’t afford a PPI?
Many PPIs are available as low-cost generics. Omeprazole 20 mg can cost under $5 per month at pharmacies like Walmart or Costco. If you’re on Medicare or Medicaid, it’s usually covered. If you’re uninsured, ask your doctor for samples or patient assistance programs. The cost of a GI bleed-hospitalization, endoscopy, blood transfusion-is thousands of dollars. Prevention is far cheaper and safer.
Can I use natural remedies like licorice or aloe vera instead of a PPI?
No. There’s no reliable evidence that herbal remedies, probiotics, or supplements prevent NSAID-steroid GI bleeding. Some, like licorice, can even raise blood pressure or interact with steroids. Stick to proven medical treatments: PPIs. Don’t risk your health on untested alternatives.
Leonard Shit
January 5, 2026 AT 12:55bro i took ibuprofen for my back and prednisone for my allergies last month and felt fine… until i woke up puking black stuff. never again. no warning, no pain, just… gone. thanks for the heads up.
Rachel Wermager
January 7, 2026 AT 03:29Let’s be clear: the COX-1 inhibition + glucocorticoid-mediated suppression of mucosal repair is a synergistic pharmacodynamic disaster. The relative risk multiplier of 12x isn’t anecdotal-it’s meta-analytically robust across multiple RCTs and cohort studies. PPIs aren’t ‘just acid reducers’-they’re mucosal protectants that upregulate prostaglandin-independent cytoprotective pathways. H2RAs? Inadequate. Antacids? Placebo-tier. The data is unequivocal.
Vinayak Naik
January 8, 2026 AT 20:40bro in india we just take ‘digene’ with every painkiller like it’s candy… i just learned i was playing russian roulette with my stomach. now i’m on omeprazole 20mg daily even after my steroid course. cheap as chai, saves your life. share this with your uncle who still thinks ‘gastric’ means ‘too much spicy food’.
Kiran Plaha
January 10, 2026 AT 07:36i never knew this was a thing. i’ve been on ibuprofen for years for my knee and just started prednisone for a flare-up. my doc never said anything. i’m gonna call them tomorrow and ask for a PPI. thanks for making me aware.
Kelly Beck
January 12, 2026 AT 04:51OMG I’M SO GLAD I READ THIS 😭 I’M ON PREDNISONE RIGHT NOW AND TOOK IBUPROFEN FOR MY PERIOD 😅 I JUST WENT TO MY PHARMACY AND GOT OMEPRAZOLE 20MG FOR $5!! THANK YOU FOR SAVING ME FROM A NIGHTMARE 🙏❤️ YOU’RE A LIFESAVER 🌟
Katie Schoen
January 13, 2026 AT 22:45so let me get this straight… doctors are literally prescribing a combo that’s basically a chemical landmine… and then acting surprised when people bleed out? 🤦♀️ and we wonder why people don’t trust the system. ppi’s should be auto-added at the pharmacy level. no exceptions. no ‘but i feel fine’ nonsense.
Beth Templeton
January 14, 2026 AT 18:05PPIs work. End of story. Stop giving H2 blockers like they’re a real option. You’re not helping. You’re just saving pennies and risking lives.
Wesley Pereira
January 15, 2026 AT 01:04the fact that 68% of Kaiser patients got protected but only 32% of community clinics did… that’s not a clinical gap. that’s a class gap. poor people get Tums. rich people get PPIs. and the system calls it ‘care’.
Molly McLane
January 15, 2026 AT 18:25Thank you for writing this so clearly. I’m a nurse and I’ve seen too many patients come in with GI bleeds after being told ‘it’s just a short course’ or ‘take Tums if you feel funny.’ This needs to be in every primary care office. Print it out. Tape it to the counter.
Brian Anaz
January 17, 2026 AT 13:29another liberal medical propaganda piece. next you’ll tell me vaccines cause autism. people get sick because they’re weak. stop coddling them with PPIs. just tell them to stop being lazy and eat less junk.
Saylor Frye
January 19, 2026 AT 12:29It’s fascinating how the pharmacodynamics of COX-1 suppression intersects with glucocorticoid-induced inhibition of fibroblast proliferation and angiogenesis. The epistemological irony is that we’ve known this since the 1990s, yet clinical inertia persists due to cognitive dissonance in primary care. A true case study in the pathology of medical complacency.
Matt Beck
January 20, 2026 AT 02:09we are all just stardust… and stomach lining… and NSAIDs… and PPIs… 😔💔 the universe gave us pain… and then gave us a way to heal… but we forgot how to listen… 🌌💊 maybe the real problem isn’t the drugs… it’s that we stopped caring about our bodies… until they screamed…