Stroke Types: Ischemic vs. Hemorrhagic and How to Prevent Them
Every 40 seconds, someone in the U.S. has a stroke. And every 4 minutes, someone dies from one. But here’s the thing: stroke isn’t just one thing. It’s two very different emergencies with different causes, symptoms, and treatments. Knowing the difference isn’t just academic-it could save your life or someone else’s.
What Exactly Is a Stroke?
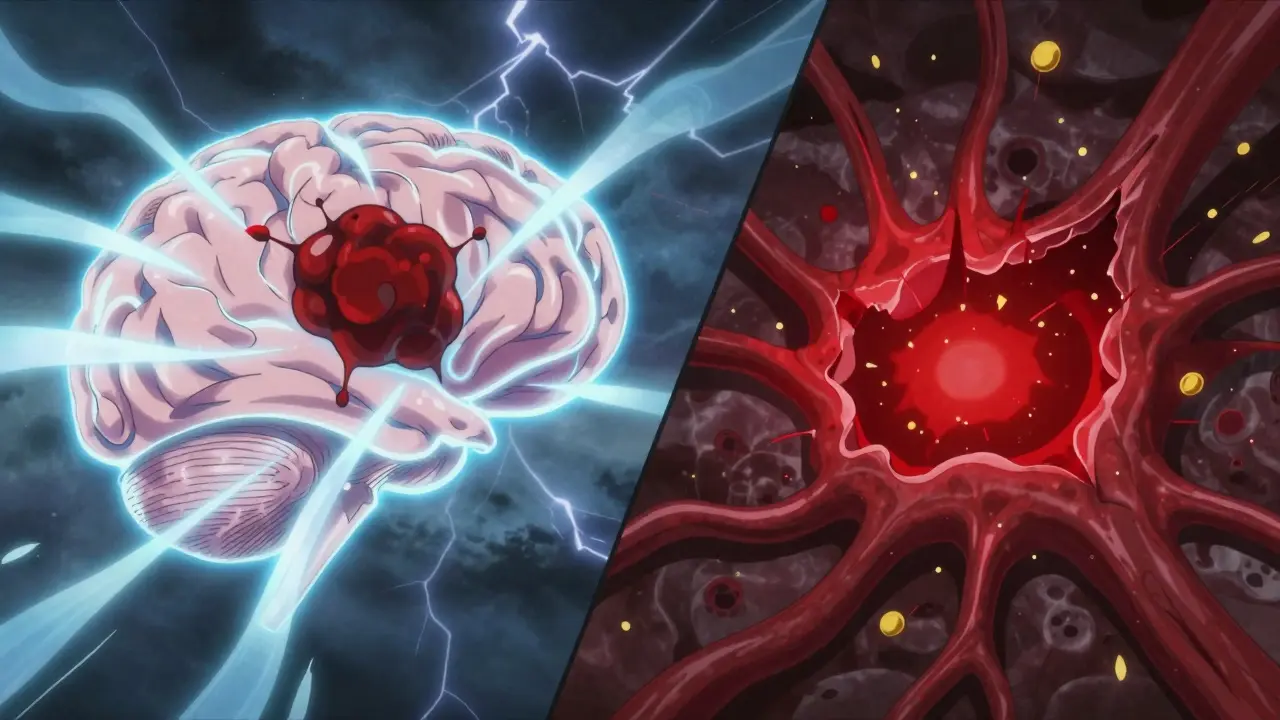
A stroke happens when blood flow to part of the brain stops. Without oxygen, brain cells start dying. The faster you act, the less damage happens. But you can’t treat all strokes the same way. Two main types make up nearly all cases: ischemic and hemorrhagic.Ischemic Stroke: The Blockage
About 87% of all strokes are ischemic. That means something is blocking a blood vessel in your brain. Think of it like a clogged pipe. The blockage can be a clot that forms right there in the brain (called a thrombotic stroke), or one that travels from elsewhere-like your heart-and gets stuck (embolic stroke). About 30% of ischemic strokes have no clear cause, even after full testing. These are called cryptogenic strokes. The symptoms usually come on slowly. You might notice numbness in your arm or leg that gets worse over 10 to 20 minutes. Your speech might slur. You might feel dizzy or confused. It’s easy to brush off as fatigue or a migraine. But if you wait too long, the damage becomes permanent.Hemorrhagic Stroke: The Burst
Hemorrhagic strokes make up about 13-15% of cases, but they’re more deadly. Instead of a blockage, a blood vessel bursts. Blood leaks into or around the brain, creating pressure that crushes brain tissue. There are two kinds: intracerebral hemorrhage (bleeding inside the brain) and subarachnoid hemorrhage (bleeding on the brain’s surface, often from a ruptured aneurysm). This type hits fast. People often describe it as the worst headache of their life-like being hit in the head with a sledgehammer. Nausea, vomiting, seizures, and sudden loss of consciousness are common. One study found 92% of hemorrhagic stroke patients had a severe headache, compared to just 19% in ischemic cases. Pupils may dilate unevenly. One side of the face might droop faster. Agitation or confusion can come on instantly.Why the Difference Matters
Treatment for ischemic and hemorrhagic strokes is completely opposite. Give a clot-busting drug like tPA to someone with a bleed, and you make things worse-possibly fatal. That’s why the first thing doctors do is a CT scan. It shows whether there’s bleeding or not. For ischemic strokes, if you get to the hospital within 3 to 4.5 hours, you might get tPA or tenecteplase to dissolve the clot. For larger clots, a mechanical thrombectomy-a procedure where a device physically pulls the clot out-can work up to 24 hours after symptoms start. Many hospitals now use AI tools like Viz.ai to spot strokes on scans faster, cutting treatment delays by over 50 minutes. For hemorrhagic strokes, the goal is to stop the bleeding and reduce pressure. Surgery might be needed. Clipping an aneurysm with a metal clip or coiling it with tiny wires can prevent re-bleeding. New techniques, like minimally invasive surgery with clot-dissolving drugs, have reduced death rates by 10% in recent trials.
What Causes Each Type?
Ischemic strokes are linked to heart and artery problems. Atrial fibrillation-where the heart beats irregularly-is a big one. It lets blood pool and clot. People with AFib have five times the stroke risk. High cholesterol, smoking, and diabetes also contribute by clogging arteries over time. Hemorrhagic strokes are mostly about high blood pressure. Around 80% of brain bleeds happen because years of uncontrolled hypertension weaken small arteries. Even if you feel fine, high blood pressure is silently damaging your vessels. A 2021 study showed keeping systolic pressure below 120 mmHg (instead of the old 140) cut hemorrhagic stroke risk by 38%.Prevention: What Actually Works
You can’t prevent every stroke, but you can cut your risk dramatically. For ischemic stroke prevention:- If you have atrial fibrillation, take anticoagulants like apixaban or warfarin. They reduce stroke risk by 60-70%.
- Take low-dose aspirin or clopidogrel if you’ve had a prior stroke or TIA. It lowers recurrence by 25%.
- Manage cholesterol. Statins don’t just lower LDL-they stabilize plaque in arteries, making clots less likely.
- Control your blood pressure. This is the #1 thing you can do. Check it regularly. If it’s above 130/80, talk to your doctor.
- Avoid heavy alcohol and cocaine. Both spike blood pressure and trigger bleeds.
- If you have an unruptured aneurysm, your doctor may monitor it or recommend surgery depending on size and location.
- Quit smoking. Your stroke risk drops by half within a year.
- Move more. 150 minutes a week of brisk walking cuts overall stroke risk by 27%.
- Eat like a Mediterranean diet-lots of vegetables, olive oil, fish, nuts, and whole grains. The PREDIMED study showed a 30% lower stroke risk with this pattern.
- Lose weight if you’re overweight. Even 5-10% loss improves blood pressure and heart rhythm.
Recognizing the Signs-FAST Is Still the Best Tool
You don’t need to know the difference between ischemic and hemorrhagic to save a life. Just remember FAST:- Face drooping: One side of the face sags or feels numb. Ask the person to smile.
- Arm weakness: One arm drifts down when raised. Ask them to lift both.
- Speech difficulty: Speech is slurred, strange, or hard to understand. Ask them to repeat a simple sentence.
- Time to call 911: If any of these signs are there-even if they go away-call emergency services immediately.

What Happens After a Stroke?
Recovery depends on how much brain tissue was damaged, not just the stroke type. Some people with large ischemic strokes recover well. Others with small bleeds have lasting problems. Rehabilitation-physical therapy, speech therapy, occupational therapy-is critical. The sooner you start, the better. Many stroke survivors struggle with depression, fatigue, or memory issues. Support groups help. Online communities like Reddit’s r/stroke show that people who stay active in recovery programs have better outcomes.What’s New in Stroke Care?
Science is moving fast. A 2023 study showed that a simple blood test measuring GFAP-a protein released when brain cells are damaged-can tell if a stroke is hemorrhagic or ischemic within 15 minutes. That could mean faster decisions in ambulances or rural clinics. MRI scans are now being used to find brain tissue that’s still salvageable, even hours after symptoms start. The WAKE-UP trial showed some patients could safely get clot-busting drugs up to 9 hours after onset, if imaging showed they still had good brain tissue left. Telestroke networks are expanding. In rural areas, a neurologist can video-call into a local ER and guide treatment in real time. Since 2018, access to specialists has jumped 300% in these areas.Final Thoughts
Stroke isn’t just an old person’s disease. About 1 in 4 strokes happen in people under 65. You can’t control your age, but you can control your blood pressure, your diet, your activity level, and whether you smoke. You can learn the signs and act fast. The most dangerous myth is that if symptoms go away, it’s not a stroke. That’s a TIA-a mini-stroke-and it’s a warning sign. One in three people who have a TIA will have a full stroke within a year if they don’t act. Don’t wait for the perfect moment. Don’t call a family member first. Don’t drive yourself to the hospital. Call 911. Time is brain. And every second counts.Can a stroke happen to someone young?
Yes. About 25% of strokes occur in people under 65. Risk factors like high blood pressure, obesity, smoking, and atrial fibrillation are rising in younger adults. Even without classic risk factors, conditions like patent foramen ovale (a heart defect) or blood clotting disorders can cause strokes in teens and 20-somethings.
Is it possible to have a stroke and not know it?
Yes. Silent strokes happen when small vessels are blocked or bleed in less critical areas. People might feel slightly off, forgetful, or unsteady-but not enough to seek help. These often show up on brain scans done for other reasons. Over time, multiple silent strokes can lead to memory loss or dementia.
Do all strokes require surgery?
No. Most ischemic strokes are treated with medication, not surgery. Only large clots may need mechanical thrombectomy. Hemorrhagic strokes sometimes need surgery to stop bleeding or remove clots, but many are managed with medication to control pressure and blood pressure. Surgery is reserved for specific cases, like large bleeds or ruptured aneurysms.
Can you prevent a second stroke?
Absolutely. The risk of a second stroke is highest in the first year after the first one. But taking prescribed medications-like blood thinners, blood pressure pills, or statins-along with lifestyle changes, can cut that risk by more than half. Regular follow-ups with a neurologist or stroke clinic are key.
Why is high blood pressure so dangerous for stroke?
High blood pressure wears down the walls of small arteries in the brain. Over time, they become brittle and prone to rupture, causing hemorrhagic strokes. It also speeds up atherosclerosis, leading to clots that cause ischemic strokes. Keeping pressure below 120/80 is the most effective way to prevent both types.
Is aspirin safe to take every day to prevent stroke?
Only if your doctor says so. Daily aspirin can help prevent a second stroke or heart attack in people with known cardiovascular disease. But for healthy people without risk factors, the risk of internal bleeding may outweigh the benefits. Never start daily aspirin without medical advice.
Can stress cause a stroke?
Stress doesn’t directly cause a stroke, but it raises blood pressure and can trigger unhealthy habits-like overeating, smoking, or skipping meds-that do. Chronic stress also increases inflammation, which damages blood vessels. Managing stress through sleep, exercise, or therapy is part of stroke prevention.
Dan Mack
January 15, 2026 AT 08:09Gloria Montero Puertas
January 15, 2026 AT 12:17Mike Berrange
January 16, 2026 AT 10:21Niki Van den Bossche
January 18, 2026 AT 05:16Jan Hess
January 19, 2026 AT 08:23Diane Hendriks
January 20, 2026 AT 01:12Frank Geurts
January 21, 2026 AT 13:54Arjun Seth
January 22, 2026 AT 08:15Sohan Jindal
January 22, 2026 AT 10:29