Tapering Opioids Safely: How to Reduce Side Effects and Avoid Withdrawal
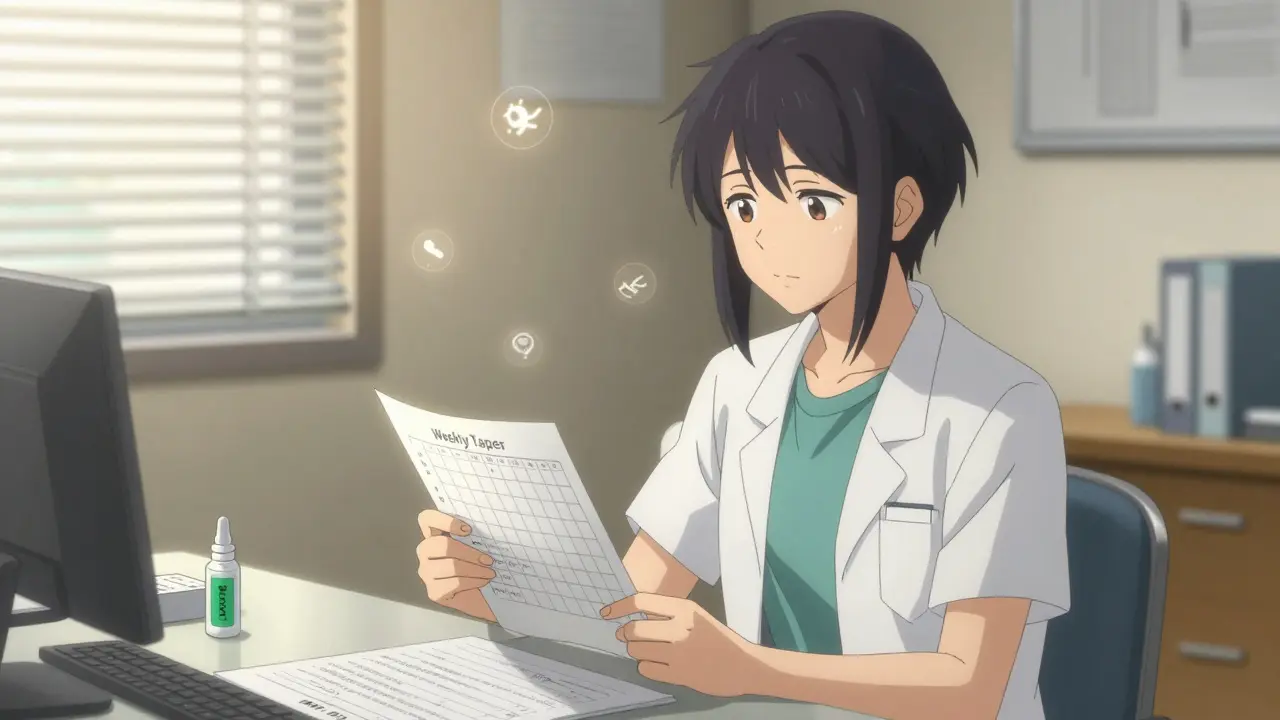
Opioid Tapering Calculator
Safe Tapering Calculator
Your Safe Tapering Schedule
Current Dose: MME
Taper Speed:
Frequency:
Maximum Safe Reduction: MME per cycle
Estimated Timeline:
| Cycle | New Dose | Start Date | End Date |
|---|
Stopping opioids suddenly can be dangerous. For people who’ve been taking them for weeks or months, the body adapts. When the drug is removed too fast, it doesn’t just hurt-it can trigger panic, vomiting, muscle spasms, and even suicidal thoughts. That’s why opioid tapering isn’t about cutting pills. It’s about planning a slow, safe exit with your doctor’s help.
When Should You Consider Tapering?
Opioids aren’t meant for long-term pain control. If you’ve been on them for more than three months and your pain hasn’t improved, it’s time to talk about alternatives. Same goes if you’re feeling foggy all day, constipated all the time, or if your doctor notices you’re asking for refills too early. Other red flags: mixing opioids with sleep aids or anxiety meds, having a past overdose, or feeling hopeless.
The CDC says abrupt discontinuation is never okay. Between 2012 and 2017, the FDA recorded over 100 cases where people were cut off cold turkey-many ended up in the ER or attempted suicide. That’s why every opioid prescription label now has a warning: Do not stop suddenly if you’re dependent.
How Fast Should You Taper?
There’s no one-size-fits-all speed. But here’s what the evidence shows:
- For most people: Reduce by 10% to 25% every 2 to 4 weeks.
- For high-dose users (over 90 morphine milligram equivalents daily): Slow it down to 5% to 10% per month.
- Never go faster than 25% per week-especially if you’re on benzodiazepines or have depression.
A 2021 study found patients who lost more than 10% of their dose per week had a 68% higher risk of overdose and a 78% higher risk of self-harm. That’s not a risk worth taking.
Most patients prefer slower tapers. In a 2022 survey of 1,200 people, 63% wanted to cut by 10% each month. Only 9% wanted to go faster than 20% per week-and those who did were far more likely to quit the plan entirely.
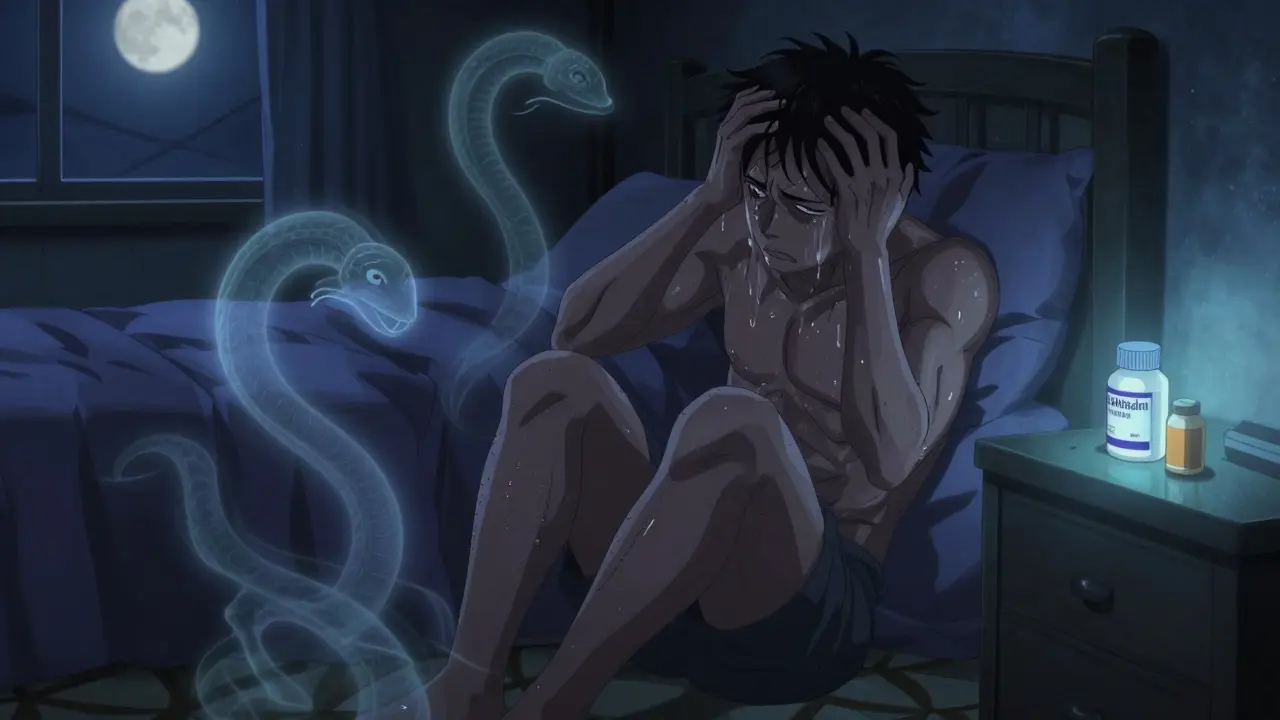
What Happens During Withdrawal?
Withdrawal isn’t just discomfort. It’s your nervous system screaming for the drug it’s been relying on. Common symptoms include:
- Anxiety (82% of people report this)
- Insomnia (76%)
- Muscle aches and cramps (68%)
- Diarrhea and nausea (59%)
- Sweating, chills, and runny nose
These usually peak within the first week and start to fade after 2 to 3 weeks. But the emotional toll-restlessness, irritability, low mood-can last longer. That’s why support isn’t optional. It’s essential.
Medications That Help During Tapering
You don’t have to suffer through this alone. Doctors can prescribe non-opioid tools to ease the ride:
- Clonidine (0.1-0.3 mg twice daily): Reduces sweating, anxiety, high blood pressure, and rapid heartbeat.
- Hydroxyzine (25-50 mg at bedtime): Calms nerves and helps you sleep.
- Loperamide (2-4 mg as needed): Stops diarrhea without the opioid high.
- NSAIDs or acetaminophen: For lingering pain. No opioids needed.
For people with a history of opioid misuse or mental health struggles, buprenorphine may be added. It’s not a replacement-it’s a bridge. A 2021 JAMA study showed combining it with therapy dropped taper failure rates from 44% to just 19% over six months.
Why Patient Agreement Matters
Tapering fails when it feels forced. The CDC found that when patients were part of the decision, discontinuation rates dropped by 47%. That’s huge.
Successful tapers almost always start with a conversation: “What are your goals?” “What’s your biggest fear?” “What would make this feel safer?”
Many people don’t want to quit opioids entirely-they just want to feel better. One study found 68% of successful tapering plans aimed for lower doses, not zero. Maybe you’ll end up on half your original dose, but sleep through the night, walk without pain, and stop feeling like you’re drugged all day. That’s progress.
What to Avoid
Don’t let fear drive the process. Between 2017 and 2020, 12% of primary care doctors misread the 2016 CDC guidelines and cut patients off abruptly. Seventeen people died by suicide as a result.
Don’t taper if you’re:
- Untreated for depression, PTSD, or anxiety
- Currently using alcohol or benzodiazepines
- Experiencing active substance use disorder
- Going through a major life crisis
These aren’t roadblocks-they’re warning signs. Tapering in the middle of a mental health crisis can make things worse. Wait until you’re stable.

Protecting Yourself: Naloxone and Documentation
If you’re on more than 50 morphine milligram equivalents daily, or you’ve had an overdose before, your doctor should give you naloxone before you even start tapering. Why? Forty-one percent of opioid deaths during tapering happen in the first 30 days. Naloxone can reverse an overdose if it happens.
Also, get it in writing. Oregon’s guidelines found that 87% of successful tapers had a signed agreement between patient and provider. It doesn’t have to be fancy. Just a note that says:
- Your current dose
- Your taper schedule
- Your symptoms to watch for
- Your emergency contact
That paper isn’t bureaucracy. It’s your safety net.
What Comes After Tapering?
Stopping opioids isn’t the end-it’s a new beginning. Most people need ongoing support:
- Cognitive behavioral therapy (CBT) helps rewire how you think about pain.
- Physical therapy rebuilds strength and movement without drugs.
- Group support reduces isolation and gives you real stories to hold onto.
People who stick with these aftercare tools are far more likely to stay off opioids long-term. One study showed that 70% of those who combined tapering with CBT and exercise reported better quality of life-even if their pain didn’t vanish completely.
Final Thoughts
Tapering opioids safely isn’t about willpower. It’s about smart planning, medical support, and listening to your body. You don’t have to go through this alone. If you’re ready to reduce your dose, ask your doctor for a plan-not just a script.
Slow is safe. Collaborative is better. And progress-no matter how small-is worth celebrating.
Emma Hooper
January 1, 2026 AT 03:08Okay but can we talk about how the real villain here isn’t opioids-it’s the system that treats chronic pain like a moral failing? I was on 60mg for 8 years after a car wreck. My doctor told me to ‘just push through’ and cut me off in 2 weeks. I ended up in the ER with seizures. Now I’m on gabapentin and yoga. Not perfect, but alive. Stop blaming patients. Fix the damn healthcare machine.
Also-clonidine is a GODSEND. I didn’t know it existed until my pain nurse slipped me a script. Why isn’t this in every primary care office?!
Harriet Hollingsworth
January 2, 2026 AT 23:52This is why people die. No one should ever be on opioids longer than 30 days. It’s addiction waiting to happen. If you can’t handle pain without drugs, maybe you’re weak. The CDC guidelines exist for a reason. Stop romanticizing dependence.
And don’t even get me started on buprenorphine-it’s just swapping one drug for another. Real recovery means total abstinence. Period.
Chandreson Chandreas
January 3, 2026 AT 05:27Man… I’ve watched my cousin go through this. He was on 120mg a day after a work injury. Took him 11 months to taper down to zero. He cried every night for 3 weeks. But now? He’s painting again. Hiking. Playing with his kid. No more fog.
It’s not about quitting pain. It’s about getting your life back. 🙏
And yeah, naloxone? Everyone should have one. Like a fire extinguisher. You hope you never need it… but you’re glad it’s there.
Darren Pearson
January 3, 2026 AT 06:42While the article presents a commendable framework for opioid tapering, it is imperative to underscore the methodological rigor required in clinical implementation. The referenced studies, particularly the 2021 JAMA publication, are methodologically sound, yet the generalizability of findings across heterogeneous populations remains underexplored. Furthermore, the reliance on self-reported survey data from 1,200 individuals introduces significant selection bias, as those who completed the survey likely represent a subset of patients with higher baseline motivation.
One must also question the omission of pharmacoeconomic analyses-how do these protocols scale in under-resourced primary care settings? Without addressing structural barriers, we risk creating a two-tiered system of care.
Stewart Smith
January 3, 2026 AT 18:42Wow. So the article says ‘slow is safe’ and then lists a 25% weekly cut as the max. That’s not slow. That’s a sprint with a parachute. I tapered at 5% a month. Took 18 months. Felt like dying for the first 6. But I didn’t OD. Didn’t quit. Didn’t cry in the shower every night.
Also-why is it that every time someone tries to help, the internet turns it into a debate about willpower? You don’t need to be a hero. You just need to not die.
Aaron Bales
January 4, 2026 AT 08:47Clonidine + hydroxyzine = your new best friends. I’ve seen this work a hundred times. No magic. Just science.
And yes-naloxone. Always give it. Even if they say they don’t need it. They will.
Also: CBT isn’t ‘therapy talk.’ It’s rewiring your brain’s pain alarm. Do it. Even if you think it’s dumb.
Lawver Stanton
January 5, 2026 AT 10:11Look, I get it. You’re trying to be helpful. But this whole ‘tapering’ thing is just a fancy way of saying ‘we’re giving up on you.’
My uncle was on 80mg for 15 years after a back injury. They told him he was ‘overusing.’ He had no insurance, no PT, no therapist. Just a letter saying his script was cut. He died three months later. Overdose. Alone. In his apartment.
And now you want to tell me ‘slow taper’ is the answer? What about the people who never had a doctor to begin with? What about the ones who got cut off because their insurance stopped covering opioids? This isn’t medicine. It’s bureaucratic cruelty dressed up in CDC bullet points.
And don’t get me started on ‘buprenorphine as a bridge.’ That’s just the pharmaceutical industry’s way of keeping you hooked on a different brand. Same addiction. Different label.
Why not just… fix the pain? Why not fund real rehab centers? Why not pay people to do physical therapy instead of pushing pills and then pulling them? We’re treating symptoms like they’re the disease.
I’m not saying don’t taper. I’m saying the whole damn system is broken. And you’re just rearranging deck chairs on the Titanic while people drown.
And for the love of God, if you’re going to write something this long, at least proofread. You missed a comma after ‘buprenorphine’ in paragraph 5. That’s embarrassing.
Sara Stinnett
January 7, 2026 AT 09:28How quaint. Another ‘compassionate’ guide to opioid tapering that ignores the fundamental truth: addiction is a choice. If you’re dependent on opioids after three months, you didn’t ‘get hurt’-you got lazy. The body doesn’t ‘adapt’-it craves. And craving is a psychological weakness.
Why are we medicating away discomfort instead of building resilience? Pain is a signal, not a sentence. If you can’t endure it, perhaps you’re unfit for modern life.
And let’s not pretend buprenorphine is a ‘bridge.’ It’s a hammock. A comfortable, government-subsidized hammock where people nap while the world moves on.
Also, ‘progress no matter how small’? That’s the language of surrender. Real strength is quitting cold turkey. I did it. You can too. If you’re willing to suffer.
And why are we even talking about ‘patient agreement’? That’s not medicine-that’s appeasement. Doctors aren’t therapists. They’re healers. Not negotiators.
Martin Viau
January 9, 2026 AT 07:59Canada’s approach is way better. We have provincial pain clinics, mandatory multidisciplinary reviews, and naloxone is distributed for free at pharmacies. No one gets cut off without a plan. Here in the US, it’s a free-for-all. You’re a number on a chart. We treat pain like a criminal offense. That’s not healthcare. That’s punishment.
Also-why are we still using morphine milligram equivalents? That metric was designed for research, not clinical decisions. It’s outdated. We need personalized dosing, not algorithmic cuts.
Robb Rice
January 11, 2026 AT 06:33Thank you for this. I’ve been tapering for 9 months. 10% a month. Still have bad days. But I slept through the night last week for the first time in 5 years.
And I’m not cured. But I’m here. And that’s enough.