Trichomoniasis and Infertility: What the Link Means for Your Health
Trichomoniasis Fertility Risk Calculator
Your Situation
Results
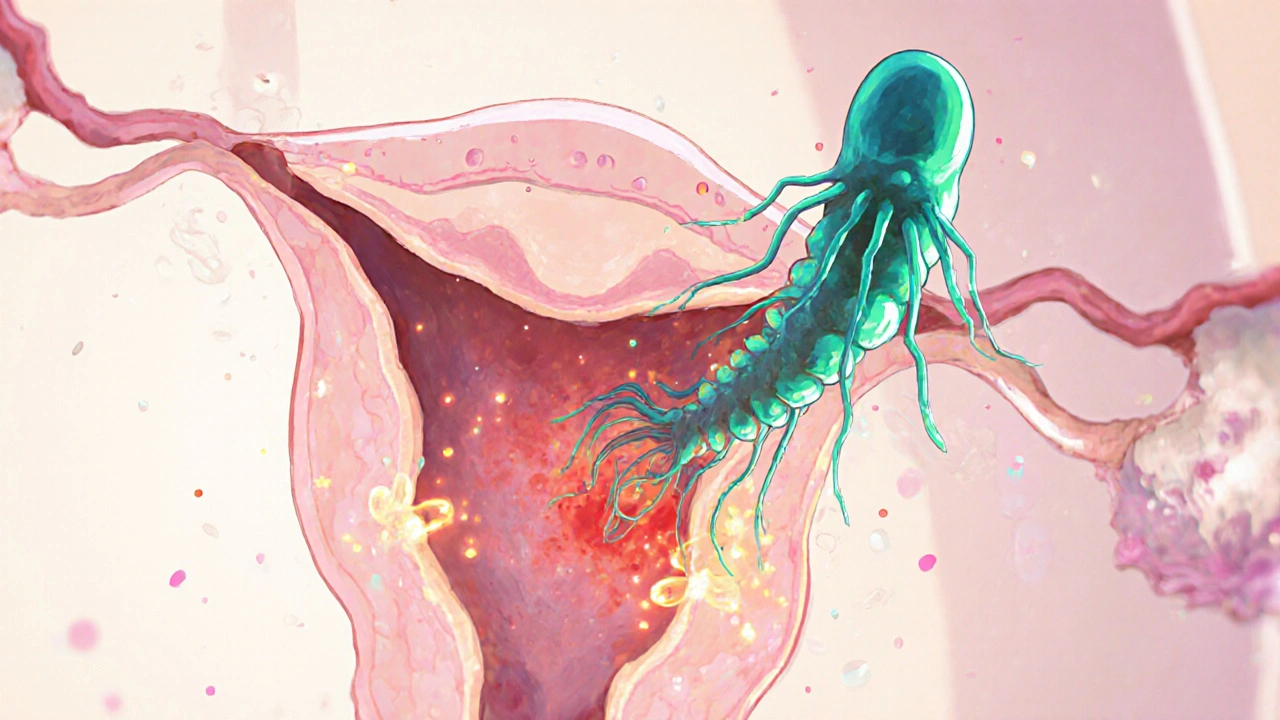
When we talk about Trichomoniasis is a common sexually transmitted infection caused by the protozoan parasite Trichomonas vaginalis, the first thing that comes to mind is often itching, discharge, or a burning sensation. What many people don’t realize is that the infection can quietly interfere with the ability to conceive. Understanding the trichomoniasis infertility link helps you spot warning signs early and take steps before a pregnancy plan is derailed.
What Exactly Is Trichomoniasis?
Trichomoniasis belongs to the group of sexually transmitted infections (STIs) known as protozoal infections. The culprit, Trichomonas vaginalis, is a single‑cell organism that thrives in warm, moist environments. It spreads through vaginal, anal, or oral sex, and in rare cases, from mother to child during childbirth.
Key facts about the infection:
- It’s the most common non‑viral STI worldwide, with an estimated 156 million new cases each year.
- Most people (about 70 %) never show symptoms, making it a silent carrier.
- When symptoms appear, they can include frothy yellow‑green discharge, vaginal odor, irritation, and painful urination.
Infertility: A Brief Overview
Infertility is defined as the inability to achieve a clinically‑recognized pregnancy after 12 months of regular, unprotected intercourse. It affects roughly 10‑15 % of couples globally and can stem from a range of male or female factors.
Common causes include hormonal imbalances, structural problems, age‑related decline, and infections. Among infections, bacterial STIs like chlamydia get a lot of attention, but protozoal infections such as trichomoniasis also play a role, especially when left untreated.
How Trichomoniasis Affects Female Fertility
Women bear the brunt of the fertility impact because the parasite directly contacts the vaginal and cervical environments. Here’s how it can hurt reproductive health:
- Inflammation of the cervix (cervicitis): The parasite’s presence triggers an immune response, leading to swelling and mucus changes that can hinder sperm movement.
- Altered vaginal microbiome: Trichomonas disrupts the balance of lactobacilli, allowing harmful bacteria to flourish. A disturbed microbiome has been linked to lower implantation rates.
- Increased risk of pelvic inflammatory disease (PID): Though PID is more commonly linked to bacterial STIs, trichomoniasis can act as a co‑factor, spreading upward to the uterus, fallopian tubes, and ovaries.
- Scar tissue formation: Chronic infection can cause scarring in the fallopian tubes, leading to blocked or damaged pathways for the egg.
- Adverse effect on embryo implantation: Inflammatory cytokines released during infection may create a hostile environment for an embryo trying to attach to the uterine lining.
Studies from 2023‑2024 that tracked over 2,000 women found that those with untreated trichomoniasis had a 22 % lower chance of conceiving within a year compared to women who tested negative.
How Trichomoniasis Impacts Male Fertility
Men are often overlooked, but the parasite can linger in the urethra and even in seminal fluid. The effects include:
- Semen quality reduction: Inflammation can lower sperm motility and increase abnormal morphology.
- Urethral irritation: Discomfort may lead to reduced frequency of intercourse, indirectly affecting conception chances.
- Transmission to partner: Even if a man shows no symptoms, he can repeatedly reinfect his partner, perpetuating a cycle of infertility risk.
A 2022 meta‑analysis of 12 cohort studies reported a modest but statistically significant 8 % drop in pregnancy rates when the male partner was a silent trichomoniasis carrier.

Diagnosing Trichomoniasis Early
Because the infection is often asymptomatic, routine screening is essential, especially for those planning a pregnancy. The most reliable tests include:
- Nucleic acid amplification test (NAAT): Detects parasite DNA with >99 % sensitivity.
- Rapid antigen test: Provides results in minutes, useful in clinics without lab facilities.
- Microscopic wet mount: Less sensitive (around 60 %) but still used in low‑resource settings.
For couples experiencing infertility, many reproductive specialists now include a comprehensive STI panel-NAAT for Trichomonas, Chlamydia, Gonorrhea, Mycoplasma genitalium, and bacterial vaginosis-as part of the initial work‑up.
Treatment Options and Their Effect on Fertility
The standard regimen remains a single dose of metronidazole or its cousin tinidazole. Both are nitroimidazole antibiotics that target the parasite’s DNA.
| Drug | Typical Dose | Success Rate | Side Effects |
|---|---|---|---|
| Metronidazole | 2 g orally, single dose | ≈ 95 % | Nausea, metallic taste, rare allergic reaction |
| Tinidazole | 2 g orally, single dose | ≈ 97 % | Headache, dizziness, less nausea than metronidazole |
| Metronidazole (7‑day course) | 500 mg twice daily for 7 days | ≈ 93 % | Higher cumulative side‑effects, better for pregnant women in second trimester |
Both drugs are safe for non‑pregnant adults, but pregnant women in the first trimester are advised to postpone treatment until the second trimester unless symptoms are severe. Importantly, successful treatment restores normal vaginal flora within 2‑3 weeks, which in turn improves the chances of conception.
Preventing Reinfection and Protecting Fertility
Even after a successful course, the parasite can bounce back if the sexual partner remains untreated. Follow these steps to keep the infection at bay:
- Ensure both partners complete the full antibiotic regimen, even if symptoms vanish.
- Abstain from sexual activity for 7 days after treatment (or as directed by a clinician).
- Use condoms consistently; they reduce transmission risk by about 70 %.
- Schedule a repeat NAAT test 3 weeks post‑treatment to confirm clearance.
- Consider regular STI screening-every 6‑12 months-if you have multiple partners or a history of STIs.

When to Seek Specialist Care
If you’ve been diagnosed with trichomoniasis and are already trying to conceive, it’s wise to see a reproductive endocrinology and infertility (REI) specialist. They can:
- Order a comprehensive semen analysis for male partners.
- Perform a hysterosalpingogram (HSG) to check for tubal blockage after infection.
- Recommend timed intercourse or intrauterine insemination (IUI) once the infection clears.
Early intervention often restores natural fertility without the need for assisted reproductive technologies.
Quick Checklist: Managing Trichomoniasis‑Related Infertility
- Get a NAAT test if you’re sexually active, even without symptoms.
- Complete the full antibiotic course; both partners must be treated.
- Retest after 3 weeks to ensure the parasite is gone.
- Use condoms for at least one month after treatment.
- Schedule a fertility evaluation if you’ve been trying >6 months.
Bottom Line
The hidden nature of trichomoniasis means many couples miss the warning sign until it shows up as difficulty getting pregnant. By staying proactive-testing, treating, and preventing reinfection-you can break the cycle and give your reproductive system the best shot at success.
Can trichomoniasis cause a miscarriage?
Yes. The inflammation and altered vaginal flora associated with trichomoniasis can increase the risk of early pregnancy loss, especially if the infection is not treated before conception.
Is it safe to take metronidazole while trying to get pregnant?
Metronidazole is considered safe for non‑pregnant adults. Most clinicians recommend completing the treatment, waiting 48 hours, and then resuming attempts to conceive. If you’re already pregnant, discuss alternative timing with your doctor.
How often should I get screened for trichomoniasis?
If you have a new or multiple partners, a test every 6‑12 months is prudent. For couples planning pregnancy, a screening before trying to conceive is highly recommended.
Can a male partner be a silent carrier?
Absolutely. Men can harbor the parasite without any symptoms, which is why both partners need treatment to prevent reinfection.
Does using condoms eliminate the risk?
Condoms dramatically lower transmission risk-by about 70 %-but they’re not 100 % foolproof. Proper use every time you have sex is essential.
Sebastian Green
October 20, 2025 AT 18:45A silent infection can sneak up on anyone trying to conceive.
Wesley Humble
November 3, 2025 AT 01:45Statistically, untreated Trichomonas vaginalis reduces conception probability by approximately 22 % (p < 0.001); thus, neglecting routine screening constitutes a non‑trivial public‑health oversight. 👩⚕️📊
Vijaypal Yadav
November 16, 2025 AT 09:45Trichomoniasis remains the most prevalent non‑viral STI worldwide, with roughly 156 million new cases annually. Because up to 70 % of infections are asymptomatic, partners often miss the diagnosis until fertility work‑ups reveal unexplained subfertility. The parasite’s tendency to incite cervical inflammation disrupts sperm transport and alters the vaginal microbiome, both of which are critical for successful implantation. Recent cohort data from 2023‑2024 show a 22 % reduction in one‑year conception rates among untreated women. Incorporating NAAT screening into pre‑conception protocols therefore addresses a hidden barrier to pregnancy.
Alex Pegg
November 29, 2025 AT 17:45I’ve seen countless clinics prioritize chlamydia while treating trichomoniasis as a footnote, yet the literature you cite is based on small cohorts and may not reflect real‑world demographics.
laura wood
December 13, 2025 AT 01:45Your checklist hits all the practical points, especially the reminder to retest after treatment. Consistent condom use and partner compliance truly cut the reinfection cycle. It’s reassuring to see evidence‑based steps laid out clearly.
Kate McKay
December 26, 2025 AT 09:45If you’re feeling overwhelmed, break the plan into weekly goals-schedule the NAAT, set a reminder for the 3‑week follow‑up, and keep a symptom journal. Small wins keep motivation high while you navigate the fertility journey.
Demetri Huyler
January 8, 2026 AT 17:45One would assume that a population aware of basic reproductive health would not need a megaphone to reiterate the obvious-that untreated infections can sabotage conception.
JessicaAnn Sutton
January 22, 2026 AT 01:45Neglecting to treat a transmissible pathogen not only compromises personal fertility but also contravenes communal responsibility; the ethical imperative is clear.
Israel Emory
February 4, 2026 AT 09:45While the data underscore a genuine risk, it’s equally important to recognize that timely treatment restores fertility in the overwhelming majority of cases; therefore, screening should be viewed as an empowering tool rather than a source of alarm.
barnabas jacob
February 17, 2026 AT 17:45FYI, the pathogen’s protozoal load (aka trophozoites) can cause sub‑clinical cervicitis; if u skip the NAAT u risk hidden dysbiosis that throws off the whole reproductive axis.