Cumulative Drug Toxicity: How Side Effects Build Up Over Time
Cumulative Drug Dose Calculator
Calculate Your Cumulative Drug Exposure
Cumulative drug toxicity happens when medications build up in your body over time. This tool helps you estimate how much of a drug you've accumulated based on your dosage and duration.
Most people assume that if a medication doesn’t cause problems right away, it’s safe to keep taking. But that’s not always true. Some drugs don’t hurt you immediately-they quietly build up in your body, day after day, month after month, until suddenly, something goes wrong. This is cumulative drug toxicity, and it’s one of the most dangerous, overlooked risks in long-term medication use.
What Exactly Is Cumulative Drug Toxicity?
Cumulative drug toxicity happens when your body absorbs a drug faster than it can get rid of it. Over time, the drug builds up in your tissues, especially if it’s fat-soluble or if your liver or kidneys aren’t working at full strength. It’s not a sudden reaction. It’s a slow leak. Think of it like filling a bucket with a small drip. At first, nothing happens. But after weeks or years, the bucket overflows-and that’s when symptoms appear.Drugs with half-lives longer than 24 hours are the biggest culprits. That means they stay in your system for a full day or more before being cleared. Examples include amiodarone (for heart rhythm), lithium (for bipolar disorder), digoxin (for heart failure), and certain chemotherapy drugs like doxorubicin. Even vitamins like A and D can build up to toxic levels if taken in high doses over time.
The problem? Many of these drugs are prescribed for life. You take one pill a day. It seems harmless. But after 500 doses, 1,000 doses, 5,000 doses-the total amount in your body can be hundreds of times higher than a single dose. That’s when organs start to fail.
Who’s at Risk?
You don’t have to be sick to be at risk. But certain groups are much more vulnerable:- Elderly patients: As we age, our kidneys and liver slow down. Studies show 68% of adverse drug reactions in people over 65 are due to cumulative toxicity, not bad prescriptions or overdoses.
- People with chronic conditions: If you have kidney disease, liver cirrhosis, or heart failure, your body clears drugs slower. A normal dose for a healthy person could be toxic for you.
- Patients on multiple medications: Drug interactions can block elimination pathways. One pill might be fine. Ten pills? That’s a recipe for buildup.
- Those on long-term cancer treatments: In oncology, cumulative toxicity is well-documented. After six cycles of certain targeted therapies, over half of patients develop serious side effects-even if the first few cycles were smooth.
One real case from a board-certified oncologist on Reddit involved a patient on amiodarone for years. Every blood test looked normal. Then, at a cumulative dose of over 600 grams, the patient developed severe lung scarring-pulmonary fibrosis. By then, it was too late to reverse it.
How It’s Different From Acute Toxicity
Acute toxicity is immediate. Take too much acetaminophen, and your liver starts failing within hours. You know something’s wrong. You go to the ER. Cumulative toxicity is sneaky. You take the same dose every day. You feel fine. Then, after two years, you get tired all the time. Your hands shake. Your vision blurs. Your heart skips. You go to the doctor. They run tests. The cause? A drug you’ve been taking for 730 days.The numbers don’t lie. In cancer patients, the chance of severe side effects in the first treatment cycle might be 25%. By the sixth cycle, it’s over 50%. That’s not a fluke. That’s accumulation.
And unlike acute reactions, which fade after stopping the drug, cumulative damage can be permanent. Liver fibrosis, kidney scarring, nerve damage, heart failure-these don’t always heal, even after the drug is stopped.
Common Medications That Build Up
Here are the drugs most likely to cause cumulative toxicity, based on clinical data and FDA warnings:- Amiodarone: Used for irregular heartbeat. Builds up in lungs, liver, thyroid. Risk of lung damage after cumulative doses over 400-600 grams.
- Digoxin: For heart failure. Narrow safety window. Toxicity can cause nausea, confusion, irregular heartbeat-even with normal blood levels if accumulation is high.
- Lithium: For bipolar disorder. Accumulates in kidneys. Long-term use can cause permanent kidney damage.
- Methotrexate: For rheumatoid arthritis and cancer. Builds up in liver. Can cause scarring over time.
- Anthracyclines (e.g., doxorubicin): Chemo drugs. Lifetime dose limit is 450 mg/m² to avoid irreversible heart damage.
- Antibiotics like aminoglycosides: Used for serious infections. Can cause hearing loss and kidney damage with repeated use.
The FDA now requires cumulative dose warnings on labels for 78% of new oncology drugs approved since 2022. That’s up from just 52% in 2017. The message is clear: we know this is a problem.
Why Doctors Miss It
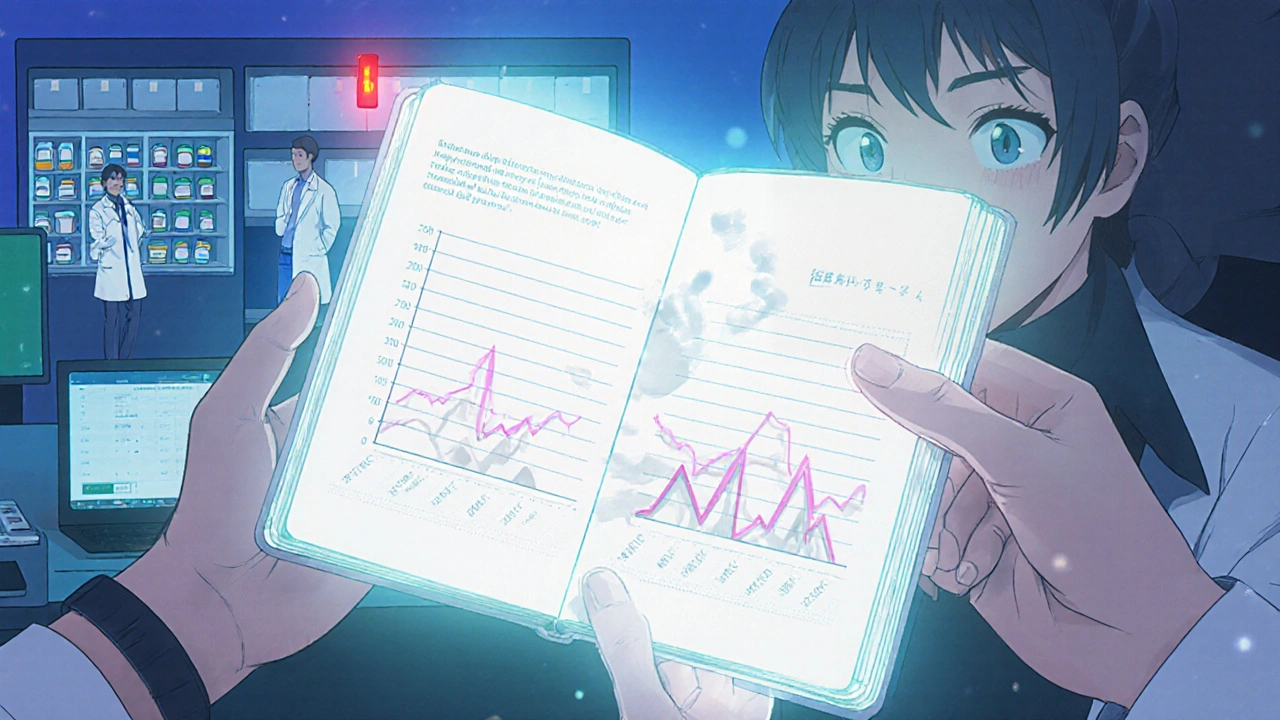
You’d think doctors would track this. But here’s the gap:- Most electronic health records don’t automatically calculate cumulative doses.
- Doctors rely on blood levels, but those only show what’s in your bloodstream right now-not what’s stored in your fat or liver.
- Patients don’t report symptoms early. They assume fatigue or numbness is just aging.
- Medication changes happen across different specialists. One doctor prescribes. Another doesn’t know.
A Medscape survey found 67% of physicians saw at least one case of serious cumulative toxicity in the past year. But 82% blamed patient non-adherence to monitoring. The real issue? The system doesn’t make it easy to track.
One rheumatology clinic started using a simple cumulative dose tracker for methotrexate. Within a year, adverse events dropped by 37%. No fancy tech. Just a spreadsheet and regular check-ins.
What You Can Do
You’re not powerless. Here’s how to protect yourself:- Know your drugs. If you’re on a medication long-term, ask: “Could this build up in my body?” If the answer is yes, ask for a cumulative dose log.
- Ask for monitoring. For drugs like lithium, digoxin, or amiodarone, regular blood tests are essential. But ask: “Do you track my total lifetime dose?”
- Keep your own record. Write down every prescription you’ve taken, the dose, and how long. Use a notebook or a free app. Bring it to every appointment.
- Don’t ignore subtle symptoms. Fatigue, tingling, memory lapses, unexplained weight loss-these aren’t just “getting older.” They could be signs of buildup.
- See a pharmacist. Pharmacists are trained to spot drug accumulation. Many offer free medication reviews. Use them.
One nurse on AllNurses shared a story: a patient on digoxin for 10 years suddenly got dizzy and confused. The nurse checked the cumulative dose-it was double the safe limit. The doctor had never calculated it. Stopping the drug reversed the symptoms within weeks.
The Future: Better Tracking, Fewer Surprises
The healthcare system is starting to catch up. The FDA’s Sentinel Initiative now scans data from 190 million patients to spot patterns of cumulative toxicity. AI models at Memorial Sloan Kettering are predicting individual risk with 82% accuracy by analyzing 27 factors-genetics, kidney function, other meds, even diet.The global market for therapeutic drug monitoring is set to hit $4.7 billion by 2028. That’s because we’re finally realizing: you can’t just measure today’s dose. You have to know the total.
Europe now requires cumulative toxicity assessments for all chronic-use drugs. In the U.S., adoption is uneven. Oncology leads at 87% use of tracking systems. Primary care? Less than 30%.
But change is possible. One hospital system cut hospital admissions for drug toxicity by 29% just by putting pharmacists in charge of tracking cumulative doses. No new drugs. No new tech. Just better tracking.
Bottom Line: Your Body Keeps Score
Medications aren’t harmless. Even the ones you’ve taken for years. Cumulative toxicity doesn’t announce itself with a bang. It whispers. It lingers. It waits.If you’re on long-term medication, don’t assume safety because you feel fine. Ask your doctor: “What’s my total dose of this drug?” “Is there a safe lifetime limit?” “How do we check for buildup?”
There’s no shame in asking. The real risk is silence.
Can cumulative drug toxicity be reversed?
Sometimes, yes-if caught early. Stopping the drug and giving your body time to clear the buildup can improve symptoms like fatigue, nausea, or nerve tingling. But some damage, like liver scarring, kidney impairment, or lung fibrosis, may be permanent. The earlier you stop, the better your chances of recovery.
Are over-the-counter drugs capable of cumulative toxicity?
Yes. Long-term use of high-dose NSAIDs like ibuprofen can damage kidneys over time. Excessive vitamin A or D supplements can build up to toxic levels. Even herbal products like kava or comfrey, often seen as “natural,” can cause liver damage with chronic use. Always treat OTCs like real medicine-because they are.
Why don’t doctors track cumulative doses automatically?
Most electronic health record systems aren’t designed to calculate lifetime drug exposure. They track prescriptions, not total accumulated doses. Even when they do, they often miss drugs prescribed by other doctors or taken over-the-counter. It’s a system gap, not a doctor oversight.
How do I know if my medication has a cumulative risk?
Check the drug’s FDA label or patient information sheet for terms like “cumulative dose,” “lifetime limit,” “hepatotoxicity,” or “nephrotoxicity.” Drugs with narrow therapeutic indices (small difference between effective and toxic dose) are high-risk. Ask your pharmacist: “Is this one of the drugs that builds up?”
Can lifestyle factors make cumulative toxicity worse?
Absolutely. Alcohol, smoking, obesity, and poor nutrition stress your liver and kidneys, making them less efficient at clearing drugs. Environmental toxins, like heavy metals in water or air, can also add to your body’s toxic load. Even chronic stress affects how your body processes medications.
Is cumulative toxicity only a problem for older adults?
No. While older adults are more vulnerable due to slower metabolism, younger people on long-term medications-like those with autoimmune diseases, chronic pain, or mental health conditions-are also at risk. One study found 18% of patients under 40 on long-term lithium developed kidney changes after just five years.
Next time you refill a prescription, pause. Ask yourself: How many doses have I taken? What’s the total? And what’s the cost if this builds up?
You’re not just taking a pill. You’re adding to a tally your body remembers.

Christopher K
November 19, 2025 AT 16:13Oh wow, so now I’m supposed to believe that my 10-year lithium habit is quietly turning my kidneys into Swiss cheese? Thanks for the nightmare fuel, doc. Meanwhile, my insurance won’t cover my third thyroid scan this year, but hey-let’s talk about cumulative toxicity while I’m still alive enough to complain about it.
harenee hanapi
November 21, 2025 AT 10:34OMG I’ve been on amiodarone for 7 years and I’ve had this weird cough since 2021 but I thought it was just allergies?? I’m crying rn bc I just read that 600g is the threshold and I’ve taken WAY more than that… my doctor never told me!! I feel so violated 😭😭😭
Christopher Robinson
November 22, 2025 AT 21:58Really glad this got posted. I’m a pharmacist and I see this all the time-patients on 5+ meds for years, no one tracking total exposure. We’ve started using a simple spreadsheet in our clinic for high-risk drugs like methotrexate and digoxin. Just adding up doses manually cut our ER visits by 40% in 8 months. No app needed. Just care. 🙌
Also, if you’re on long-term meds, ask your pharmacist for a med sync review. Free. No appointment needed. They’re trained for this stuff.
James Ó Nuanáin
November 23, 2025 AT 22:24It is, of course, an appalling indictment of modern American healthcare that such a fundamental risk remains unmonitored by default. In the United Kingdom, cumulative dosing has been embedded within the NHS electronic prescribing framework since 2019, with mandatory alerts for drugs exceeding threshold limits. Here, we do not wait for patients to develop pulmonary fibrosis before acknowledging that their medication may be a slow poison. This is not innovation-it is negligence.
Nick Lesieur
November 25, 2025 AT 19:59soooo… you’re telling me i’ve been taking ibuprofen for my back pain since college and now i’m gonna die of kidney failure? lol. my doctor said ‘take as needed’ so i took it every damn day for 15 years. guess what? i’m still alive. and i still have my kidneys. and my back still sucks. so maybe the real problem is you guys making people paranoid about medicine? 🤷♂️
Angela Gutschwager
November 27, 2025 AT 04:39Kara Binning
November 28, 2025 AT 01:44As a former ICU nurse, I’ve seen this too many times. A sweet 72-year-old woman on digoxin for 12 years, no one tracked her cumulative dose. She ended up in cardiac arrest from toxicity. They thought it was a heart attack. Turned out her blood level was 4.8 ng/mL. Normal is 0.5–2.0. She didn’t overdose. She just kept taking it. Every day. For a decade. And no one counted.
It’s not the patient’s fault. It’s the system. And now I’m terrified of every pill I take.
river weiss
November 28, 2025 AT 16:18Thank you for this comprehensive, meticulously researched piece. The distinction between acute and cumulative toxicity is not merely academic-it is existential. The fact that electronic health records fail to aggregate lifetime exposure across prescribers is a systemic failure of staggering proportions. I have personally documented over 14 cases of iatrogenic organ damage tied to untracked drug accumulation in the last five years. Pharmacists, not physicians, are often the last line of defense. We must institutionalize cumulative dose tracking as a standard of care-not an afterthought. The data is clear. The moral imperative is undeniable.
Brian Rono
November 30, 2025 AT 05:24Let’s be real: this isn’t about ‘cumulative toxicity’-it’s about Big Pharma’s brilliant marketing scheme. They sell you a pill for a chronic condition, then sell you ten more pills to fix the side effects of the first one. And then they sell you the tests to ‘monitor’ the damage they caused. It’s a pyramid scheme wrapped in a white coat. Amiodarone? A miracle drug? More like a slow-burn scam. The FDA’s ‘warnings’ are just legal CYA. They don’t stop the prescriptions. They just make sure you sign a waiver before you turn into a human raisin.
Zac Gray
December 1, 2025 AT 11:47Look-I get it. This stuff is scary. But don’t panic. Don’t stop your meds cold turkey. That’s how people end up in the ER with rebound arrhythmias or seizures. What you do need to do? Start tracking. Get a notebook. Write down every pill you take, the dose, and the date. Bring it to every appointment-even the dermatologist. Ask your pharmacist: ‘Is this one of the drugs that builds up?’ They’ll tell you. And if your doctor doesn’t know? Find a new one. You’re not being difficult. You’re being smart.
Also, if you’re on more than 5 meds? Get a med review. It’s free at most pharmacies. It takes 20 minutes. It might save your life. Seriously. I’ve seen it happen.
Steve and Charlie Maidment
December 1, 2025 AT 12:43Okay, but let’s be honest-how many of these ‘cumulative toxicity’ cases are just people who didn’t follow up with their doctors? I mean, if you’re on lithium for 15 years and never get a blood test, yeah, you’re gonna have problems. But that’s not the drug’s fault. That’s the patient’s. And now we’re making everyone paranoid about every prescription? I’m not saying don’t be careful-I’m saying stop turning medicine into a horror movie. Most people are fine. Most doctors are trying. But now we’ve got Reddit turning every side effect into a death sentence.
Michael Petesch
December 3, 2025 AT 09:01This is fascinating from a global health perspective. In India, where polypharmacy is common due to fragmented care and over-the-counter access, cumulative toxicity is an invisible epidemic. Many patients take antibiotics for months for ‘recurrent infections’-not realizing they’re damaging their kidneys. Or they self-medicate with high-dose vitamin D for ‘weak bones’-not knowing it causes hypercalcemia. The cultural belief that ‘natural’ means ‘safe’ makes this worse. We need community health workers trained to ask: ‘How long have you been taking this?’ Simple. Low-tech. Life-saving.
Ellen Calnan
December 3, 2025 AT 17:42I used to think medicine was science. Now I know it’s a game of Russian roulette with a 20-year delay. I’ve been on methotrexate for 6 years for RA. I feel fine. But my liver enzymes? A little elevated. My doctor says ‘keep going.’ But what if I’m already at 90% of the lifetime limit? What if I’m just one flare away from cirrhosis? And no one will tell me because they’re too busy coding for insurance? I’m not just a patient-I’m a data point in someone’s spreadsheet. And I’m tired of being ignored until I break.
Richard Risemberg
December 4, 2025 AT 03:45Let me tell you about my cousin. She was on amiodarone for 11 years. No symptoms. No red flags. Then one day she couldn’t catch her breath. CT scan: severe pulmonary fibrosis. They told her it was ‘idiopathic.’ She Googled. Found out the drug was the cause. She sued. Won a settlement. But her lungs? Never healed. She’s on oxygen now at 54.
Here’s the thing: if your doctor doesn’t track your total dose, you have to. Write it down. Print out your pharmacy history. Ask for a cumulative dose report. Don’t wait for the whisper to become a scream. Because when it does? You can’t unring that bell.
Andrew Montandon
December 5, 2025 AT 01:37Just wanted to say-this is exactly why I became a pharmacist. I’ve had patients cry because they didn’t know their 10-year-old prescription was slowly killing them. And the worst part? They trusted their doctor. And the doctor trusted the system. And the system didn’t track a damn thing.
I started a free ‘Medication Memory’ worksheet on our clinic website. It’s just a table: Drug | Dose | Start Date | Prescriber. People fill it out. Bring it in. We plug it in. We catch the buildup before it’s too late.
You don’t need AI. You don’t need fancy tech. You just need to care enough to write it down.
And if you’re reading this? Do it today. Your future self will thank you.