Prescription Writing Errors and How to Catch Them as a Patient
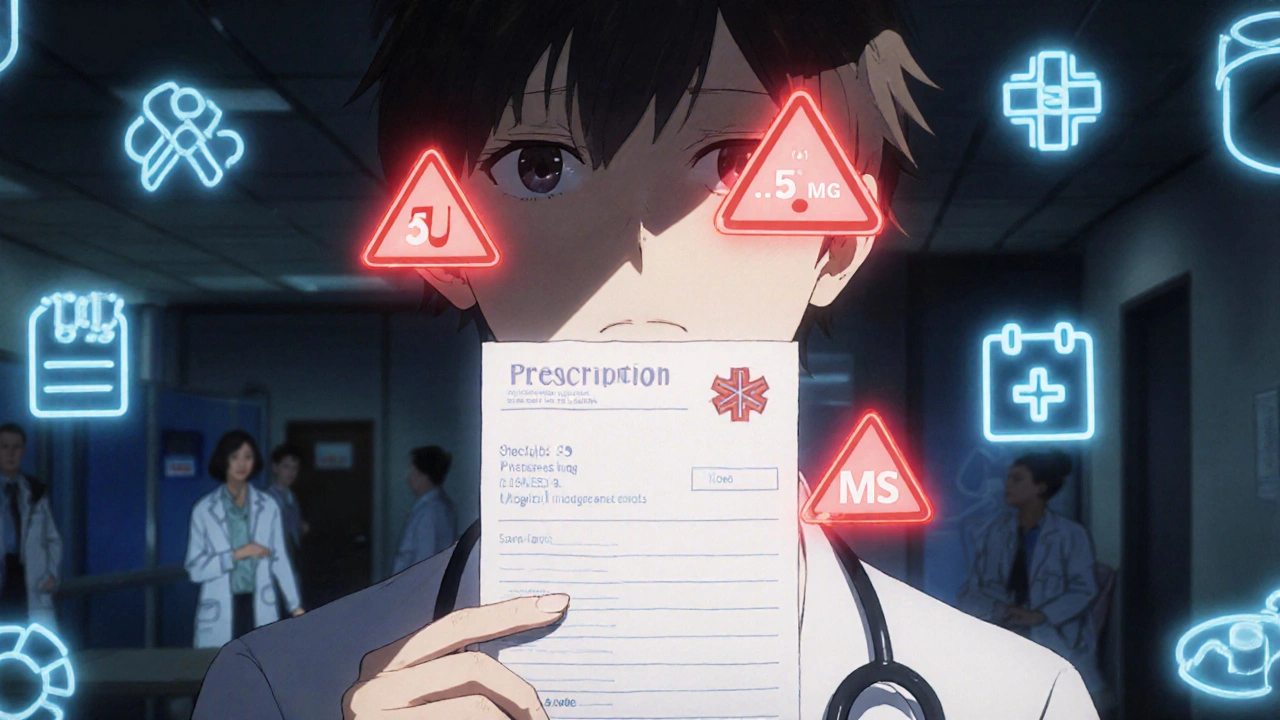
Every year, hundreds of thousands of people in the U.S. are harmed because of mistakes made when doctors write prescriptions. Some of these errors are simple-a handwritten ‘U’ for units that looks like a ‘0,’ or a decimal point missing its leading zero, turning 0.5 mg into 5 mg. Others are more complex: a drug prescribed that interacts dangerously with another, or the wrong medication entirely because ‘Zyprexa’ was confused with ‘Zyrtec.’ These aren’t rare glitches. They’re common, preventable, and often go unnoticed until it’s too late.
What Exactly Counts as a Prescription Writing Error?
A prescription writing error happens when the doctor writes down a medication order incorrectly-before it even reaches the pharmacy. This isn’t about pharmacists misreading labels or patients taking pills wrong. This is about what’s written on the paper or typed into the computer. The most frequent mistakes include:- Wrong dosage-too much, too little, or the wrong unit (mg vs. mcg)
- Illegible handwriting-still a problem even in the digital age
- Wrong drug name-look-alike or sound-alike drugs like ‘Lamictal’ and ‘Lamotrigine’
- Unclear instructions-using ‘QD’ instead of ‘once daily’ or ‘BID’ instead of ‘twice daily’
- Missing purpose-no indication like ‘for high blood pressure’ or ‘for migraines’
- Trailing or missing zeros-‘5.0 mg’ can be read as ‘50 mg’; ‘.5 mg’ can be read as ‘5 mg’
- Using dangerous abbreviations-‘U’ for units, ‘MS’ for morphine sulfate (confused with magnesium sulfate), or ‘QID’ instead of ‘four times daily’
According to the Institute of Medicine, these kinds of errors affect at least 1.5 million people in the U.S. each year. And while electronic prescribing has cut down on handwriting mistakes by over half, it’s created new problems-like choosing the wrong dose from a dropdown menu because ‘5 mg’ and ‘50 mg’ are right next to each other.
High-Risk Medications Are the Most Dangerous
Not all prescriptions carry the same risk. Some drugs are called ‘high-alert medications’ because even a small mistake can kill. These include:- Insulin
- Warfarin (blood thinner)
- Hydromorphone and other strong opioids
- Heparin (anticoagulant)
- IV potassium chloride
Even though these make up only about 8% of all prescriptions, they’re behind 72% of fatal prescription errors. That’s why it’s critical to double-check these. If your doctor prescribes insulin for diabetes, make sure the dose is clearly written as ‘5 units’-not ‘5U’ or ‘.5U.’ If you’re on warfarin, confirm the strength is ‘5 mg’ and not ‘50 mg.’ A single digit can mean the difference between life and death.
What to Look for When You Get Your Prescription
You don’t need to be a doctor to catch mistakes. The FDA recommends checking seven key things on every prescription:- Full drug name-No abbreviations. ‘Metoprolol’ not ‘Lozol.’
- Precise dosage-Always written with a leading zero for decimals under 1 (‘0.5 mg’ not ‘.5 mg’). No trailing zeros (‘5 mg’ not ‘5.0 mg’).
- Clear frequency-‘Once daily’ or ‘twice daily,’ not ‘QD’ or ‘BID.’
- Total quantity-If you’re taking a pill once a day for 30 days, you should get 30 pills. Not 300.
- Purpose of the medication-Why are you taking this? ‘For anxiety’ or ‘for high cholesterol’ should be written clearly.
- Prescriber’s contact info-If the pharmacy has to call, they need a valid phone number.
- Expiration date-Prescriptions expire. If it’s been sitting for months, ask if it’s still good.
A 2022 study from the University of Michigan found that patients who used this checklist caught 63% of errors before even getting to the pharmacy. That’s more than double the rate of those who didn’t check anything.
Red Flags That Should Make You Stop and Ask
Some errors are easy to spot if you know what to look for:- ‘U’ for units-This should always be spelled out as ‘units.’
- ‘MS’ or ‘MSO4’-Could mean morphine sulfate or magnesium sulfate. These are completely different drugs. One calms pain; the other can stop your heart.
- ‘HC’ for hydrocortisone-Might be mistaken for heparin, a blood thinner.
- ‘QID’ instead of ‘four times a day’-Patients often misread this as ‘once a day.’
- ‘Lamictal’ instead of ‘Lamotrigine’-The brand name is often used on prescriptions, but the generic is safer to confirm with your pharmacist.
Also, if your prescription is for a high-alert drug, ask: ‘Is this the right dose for someone with my kidney or liver function?’ Many errors happen because doctors don’t adjust doses for older patients or those with chronic conditions.
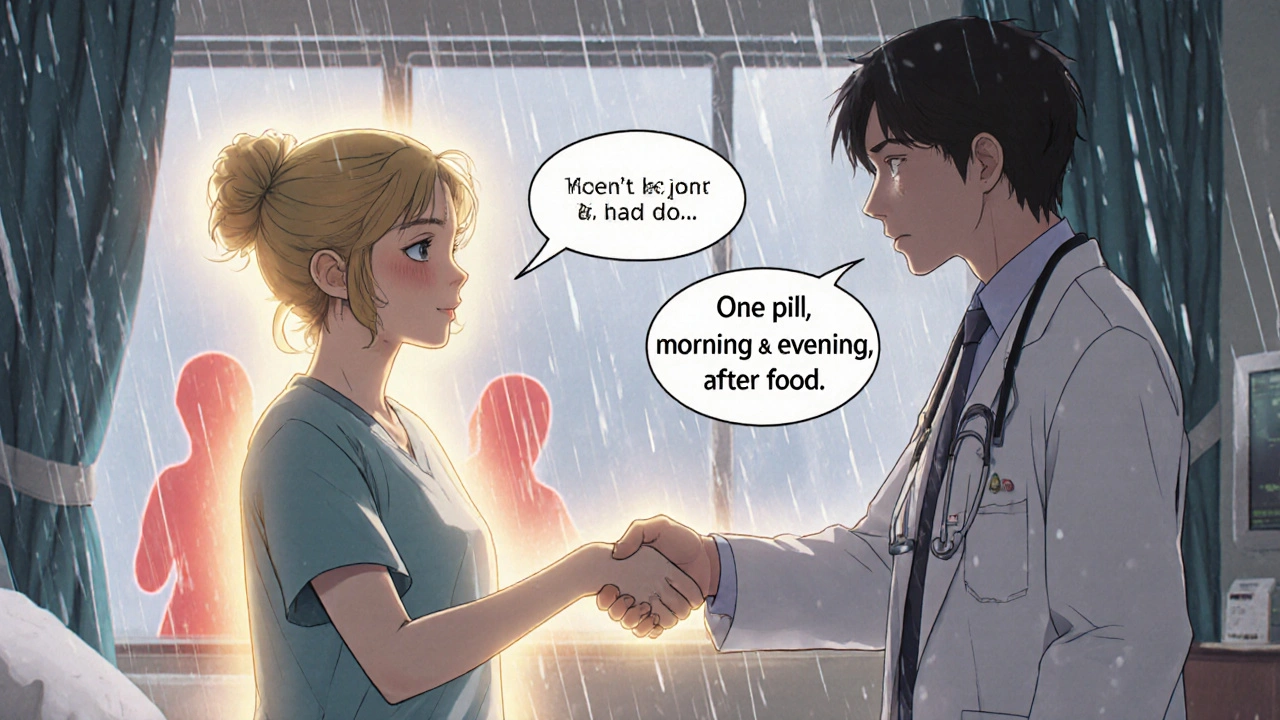
Use the Teach-Back Method to Confirm Understanding
When the doctor or nurse explains how to take your medicine, don’t just nod. Repeat it back in your own words. This is called the ‘teach-back method,’ and it’s proven to cut misunderstandings by 81%.For example: If they say, ‘Take one tablet twice a day with food,’ say, ‘So I take one pill in the morning and one in the evening, right after I eat?’ If they correct you, you’ve just caught a mistake. If they say, ‘Yes,’ you’ve confirmed you understand.
This isn’t about being difficult. It’s about being safe. A 2021 study in JAMA Network Open showed that patients who consistently asked the three ‘Ask Me 3’ questions-‘What is my main problem?’, ‘What do I need to do?’, and ‘Why is it important?’-reduced medication errors by 44%.
Verify Electronic Prescriptions Before You Leave
Even if your doctor uses an e-prescribing system, mistakes still happen. The pharmacy might get the wrong drug because the doctor clicked ‘Lisinopril’ instead of ‘Losartan’-two common blood pressure meds that look similar in dropdown menus.When you get your prescription, check the label on the bottle against what you were told:
- Does the name match?
- Is the dosage the same?
- Are the instructions clear?
Don’t assume the pharmacy caught it. Pharmacies now spend nearly 19 minutes per prescription just verifying what the doctor sent-up from 6 minutes in 2015. A lot of that time is spent fixing errors that originated with the prescriber.
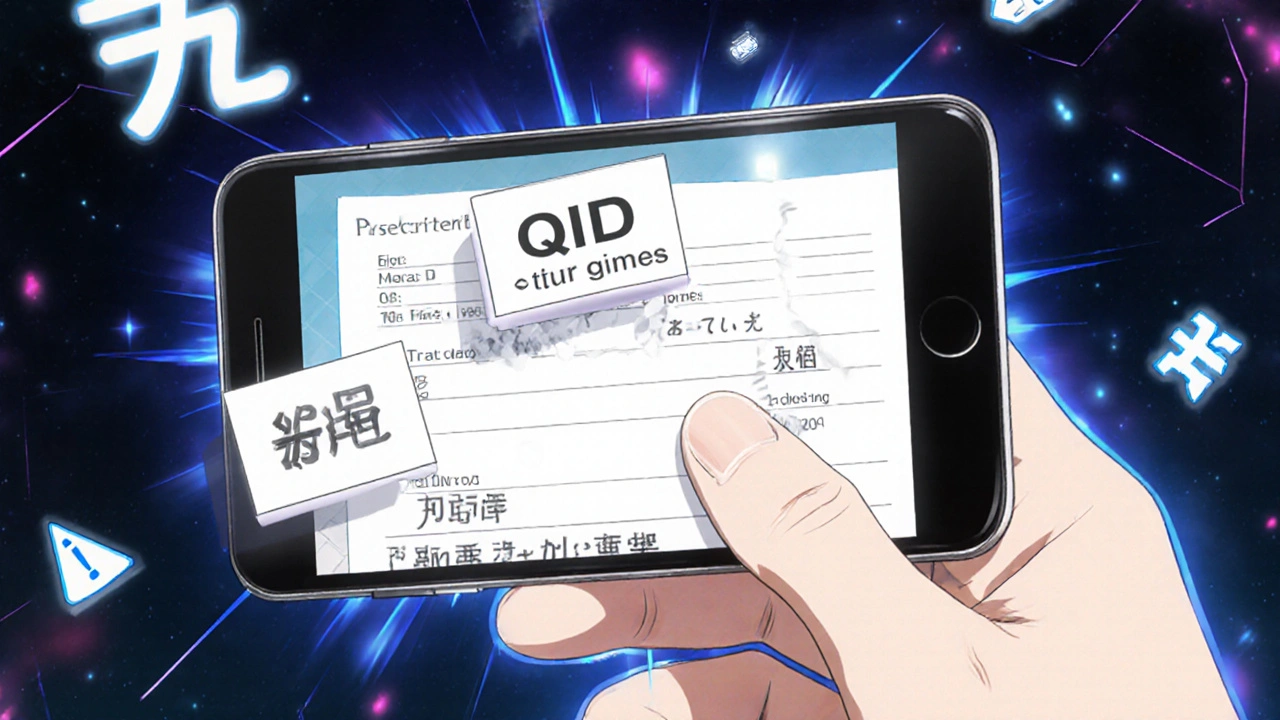
Use Technology to Help You
There are apps now that scan your prescription photo and flag potential errors. One called MedSafety, used by over 2 million people, detects things like missing zeros, dangerous abbreviations, and drug interactions. In a 2023 pilot study, it reduced patient-identified errors by 68%.Starting in 2025, all electronic health records in the U.S. will be required to give patients real-time access to their prescription details through secure apps. You’ll be able to see exactly what your doctor ordered-before the pharmacy fills it.
Some hospitals are even testing blockchain systems that create an unchangeable record of what was prescribed versus what was dispensed. If there’s a mismatch, you get an alert.
What If You Catch an Error?
If you spot something wrong, don’t panic. Don’t argue. Just say:‘I’m not sure about this. Can you double-check the dose? I think it might be 5 mg, not 50 mg.’
Most pharmacists and nurses will appreciate you catching it. In fact, they’re trained to thank you. If the pharmacy says, ‘The doctor wrote it this way,’ call the doctor’s office. Ask to speak to the nurse or the doctor directly. Have your prescription in hand and point to the error.
It’s not your job to diagnose or prescribe. But it is your job to protect your own health. The Agency for Healthcare Research and Quality says patient involvement reduces medication error risk by up to 50%.
Why This Matters More Than You Think
Prescription errors aren’t just inconvenient-they’re deadly. Between 2010 and 2020, the FDA recorded 128 deaths from simple decimal point mistakes alone. In 2023, over 21% of all medical malpractice claims were due to prescribing errors, with an average payout of nearly $300,000 per case.And yet, only 58% of doctors follow basic safety rules like avoiding abbreviations and writing full drug names. That means the burden falls on you.
You’re not being difficult by asking questions. You’re being smart. You’re doing the one thing that most patients don’t: taking responsibility for your own safety.
By the year 2027, experts predict patient-mediated error detection will become standard. But you don’t have to wait. You can start today.
What to Do Next
Here’s your simple action plan:- Always ask for the full drug name and purpose when you get a new prescription.
- Check the dosage for leading and trailing zeros.
- Never accept ‘U,’ ‘QD,’ or ‘MS’ on a prescription-ask for the full term.
- Use the teach-back method to confirm instructions.
- Compare the pharmacy label to what your doctor said.
- Download a prescription-checking app like MedSafety.
- If you’re on insulin, blood thinners, or strong pain meds, double-check everything.
Medication errors are preventable. But they won’t be fixed unless patients speak up. You have more power than you think. Use it.

Patrick Goodall
November 24, 2025 AT 23:46Kaylee Crosby
November 26, 2025 AT 04:05Mariam Kamish
November 27, 2025 AT 12:33Emma Hanna
November 29, 2025 AT 11:59Karen Ryan
November 30, 2025 AT 15:21Lawrence Zawahri
December 2, 2025 AT 07:36Benjamin Gundermann
December 2, 2025 AT 12:04Dirk Bradley
December 4, 2025 AT 05:51Adesokan Ayodeji
December 4, 2025 AT 16:11Manish Pandya
December 5, 2025 AT 21:45