GLP-1 Agonists and Gallbladder Disease: Recognizing Abdominal Pain Red Flags
GLP-1 Agonist Gallbladder Symptom Checker
Check Your Symptoms
Identify potential gallbladder issues while taking GLP-1 agonists like Ozempic, Wegovy, or Saxenda
Risk Assessment Results
Key Recommendations
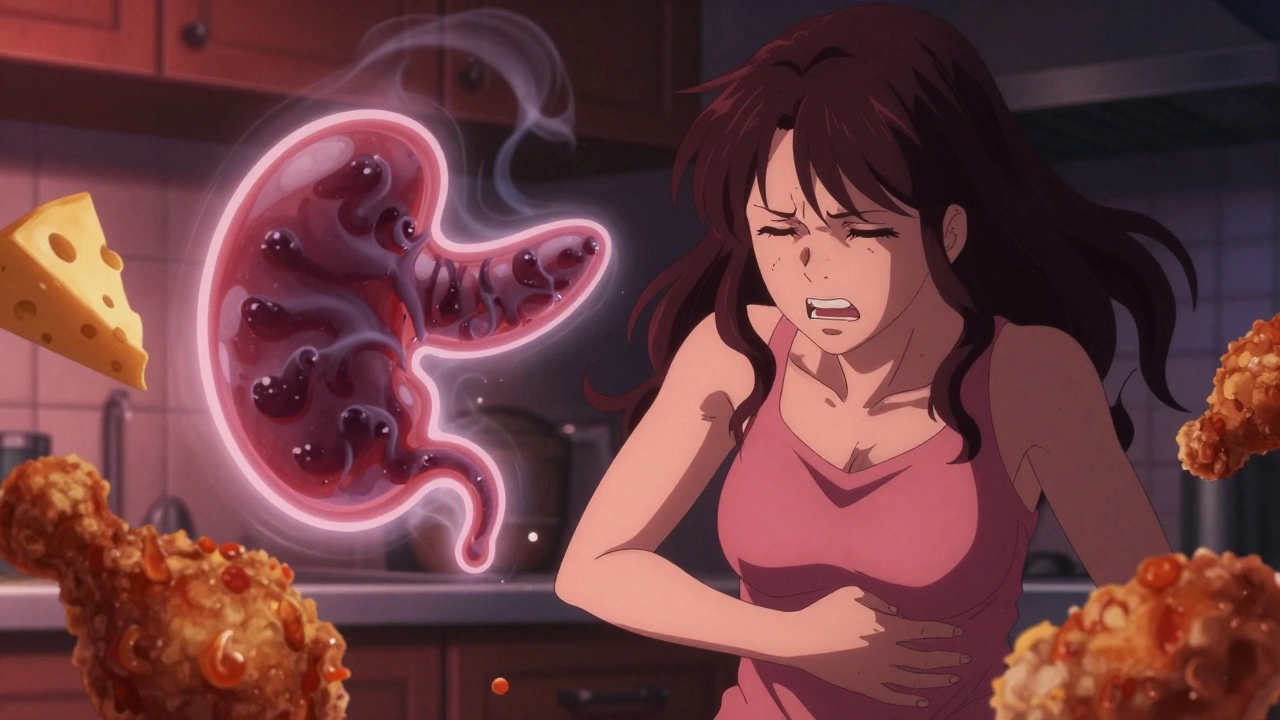
When you start taking a GLP-1 agonist like Ozempic or Wegovy, the goal is clear: better blood sugar control, weight loss, and improved health. But for some, a quiet warning sign appears - a dull, persistent ache under the right ribs that doesn’t go away after eating. It’s not just indigestion. It could be your gallbladder screaming for attention.
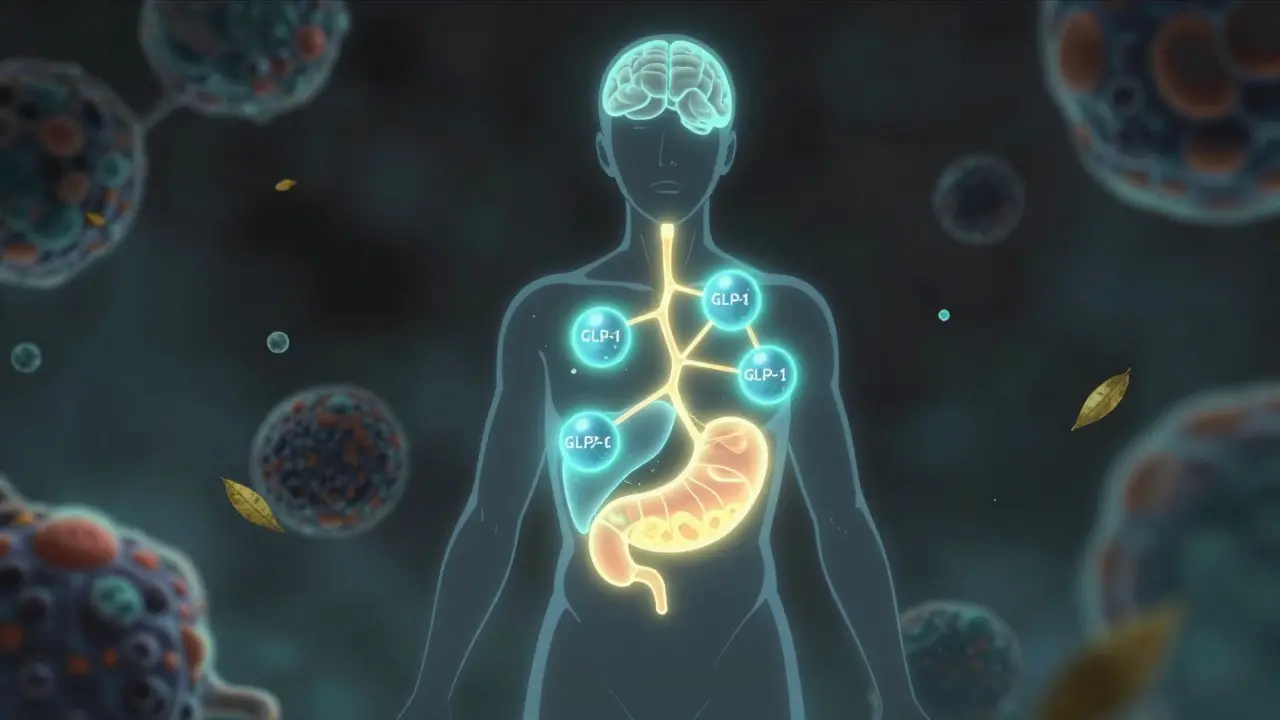
Why GLP-1 Agonists Put Your Gallbladder at Risk
GLP-1 agonists work by mimicking a hormone your body naturally makes after eating. They slow digestion, reduce appetite, and help your pancreas release insulin. But there’s a side effect most people don’t talk about: they also slow down your gallbladder. Your gallbladder stores bile, the fluid your liver makes to digest fat. When you eat something fatty, your body releases a hormone called cholecystokinin. That tells your gallbladder to squeeze and dump bile into your small intestine. GLP-1 agonists block that signal. Without that squeeze, bile sits still. And when bile sits still, it thickens. Over time, it can form sludge - then stones. A 2022 meta-analysis of 76 clinical trials involving over 56,000 people found that those taking GLP-1 agonists had a 37% higher risk of gallbladder or biliary disease compared to those on placebo. The risk wasn’t the same for everyone. People using higher doses for weight loss - like semaglutide 2.4 mg (Wegovy) or liraglutide 3.0 mg (Saxenda) - had nearly three times the risk of those using lower doses for diabetes. Liraglutide showed the highest relative risk among all GLP-1 agonists. Semaglutide wasn’t far behind. Even exenatide, the first drug in this class, carried a smaller but still present risk. The data doesn’t lie: the more weight you lose on these drugs, the more your gallbladder pays the price.The Red Flags: What Abdominal Pain Really Means
Not every belly ache is serious. But if you’re on a GLP-1 agonist and you feel this kind of pain, don’t ignore it:- Right upper quadrant pain - sharp or dull, right under your ribs, lasting more than 30 minutes. This is the most common sign. Studies show 89% of people with acute cholecystitis have this exact pattern.
- Pain that radiates to your right shoulder - it feels like your shoulder is aching, but it’s actually your gallbladder sending signals through nerves that cross paths.
- Pain after eating fatty food - tacos, cheese, fried chicken, buttered toast. These trigger the gallbladder to contract, but if it’s blocked by a stone, it hurts badly. This happens in 94% of true biliary colic cases.
- Nausea or vomiting with the pain - not just feeling queasy. This combination raises the chance of gallbladder inflammation by nearly four times.
Who’s Most at Risk?
It’s not random. Certain people are far more likely to develop gallstones on these drugs:- Women over 40 - hormonal factors make them four times more likely to form gallstones naturally. GLP-1 agonists amplify that risk.
- People with obesity (BMI over 30) - fat tissue changes how bile is made and stored. Rapid weight loss from GLP-1 drugs makes bile even more prone to crystallizing.
- Those losing weight faster than 1.5 kg per week - the faster you drop pounds, the more bile sludge builds up. Experts now recommend slowing weight loss to 0.5-1 kg per week if you have risk factors.
- Anyone with prior gallstones or gallbladder disease - if you’ve had them before, GLP-1 agonists can cause existing stones to move and block ducts. That’s when things turn dangerous fast.
What Happens When You Ignore the Pain?
Too many people think, “It’s just a side effect. I’ll tough it out.” That’s how a simple gallstone becomes a medical emergency. In the Woronow case series, 93% of gallbladder attacks happened within the first year of taking GLP-1 agonists. Most patients didn’t realize what was happening until they ended up in the ER with fever, jaundice, or sepsis. One patient, a 52-year-old woman on Wegovy, lost 30 pounds over six months. Then, after eating a cheeseburger, she had severe pain for five hours. She was diagnosed with acute cholecystitis. Two days later, she had her gallbladder removed. Online patient forums are full of similar stories. On Reddit’s r/Obesity, over 25% of users who reported abdominal pain after starting GLP-1 drugs were later confirmed to have gallstones or inflammation. Many described sudden, intense pain that came out of nowhere - often after meals they used to enjoy. The bottom line: if you’re on one of these drugs and you feel persistent, post-meal pain in your upper right abdomen - don’t wait. Don’t take antacids and hope it goes away. Get an ultrasound. Now.What If You Already Had Your Gallbladder Removed?
Good news: if you’ve had a cholecystectomy, your risk of gallstone complications from GLP-1 agonists drops dramatically. Without a gallbladder, there’s no storage for bile to turn to sludge. You won’t get gallstones. There’s still a tiny risk - maybe 1% - of residual stones or sludge getting stuck in the bile ducts. But it’s rare. Most experts agree that patients without a gallbladder can use GLP-1 agonists safely, even at high doses. Still, if you’ve had surgery and you’re starting one of these drugs, mention it to your doctor. They’ll know to watch for other signs of bile duct issues, like yellowing skin or dark urine.
What Should You Do If You’re on a GLP-1 Agonist?
Here’s what to do right now - no matter how long you’ve been on the drug:- Know your risk factors. Are you a woman over 40? Do you have obesity? Have you lost more than 1.5 kg per week? If yes, you’re in a higher-risk group.
- Learn the red flags. Right upper pain + fatty food + nausea = call your doctor. Don’t wait for fever or jaundice.
- Get an ultrasound if you have symptoms. Ultrasound is quick, painless, and 95% accurate at spotting gallstones. No radiation. No fasting needed.
- Don’t stop the drug without talking to your doctor. GLP-1 agonists reduce heart attacks and strokes in people with diabetes. The benefits often outweigh the risks - if you’re monitored.
- Slow down weight loss if you’re losing too fast. Aim for 0.5-1 kg per week. Slower loss = less bile sludge.
Linda Migdal
December 2, 2025 AT 23:53Let’s be real-Big Pharma knew this was coming. They pushed GLP-1 agonists like weight-loss magic bullets while burying the gallbladder risk in footnotes. 37% higher incidence? That’s not a side effect, that’s a design flaw. And now we’re seeing ER visits spike because patients aren’t warned until it’s too late. This isn’t science-it’s profit-driven negligence.
Women over 40? Obese? Losing weight fast? You’re basically signing a waiver for cholecystectomy. No baseline ultrasound? No informed consent? That’s malpractice waiting to happen.
The FDA label update? Too little, too late. By the time they added it, thousands were already in pain. They should’ve mandated imaging before prescription. Period.
And don’t get me started on how doctors still treat this like ‘just indigestion.’ You wouldn’t ignore chest pain and call it heartburn. Why treat abdominal red flags any differently?
This isn’t about fearmongering. It’s about accountability. If you’re prescribing this, you owe your patient an ultrasound. Not a pamphlet. Not a ‘maybe.’ An ultrasound. Now.
Tommy Walton
December 4, 2025 AT 20:42Existential question: if your gallbladder dies so your waistline can live… was it worth it? 🤔
GLP-1s are the modern-day Faustian bargain-lose 30 lbs, gain a scar. The body doesn’t ‘reward’ weight loss. It retaliates. Bile sits. Stones form. Gallbladder screams. You? You just wanted to fit into your jeans again.
Meanwhile, the universe laughs as you pop antacids like candy. 😂
Cholecystectomy isn’t a complication-it’s the *unavoidable* epilogue of metabolic arrogance. We wanted to hack biology. Now biology’s hacking us back.
James Steele
December 6, 2025 AT 04:06Let’s deconstruct the pathophysiology here, shall we? GLP-1 agonists inhibit cholecystokinin-mediated gallbladder contraction → bile stasis → cholesterol supersaturation → nucleation → sludge → stones. It’s not magic. It’s biochemistry on autopilot.
The real tragedy? The literature’s been screaming this for years. A 2022 meta-analysis? Please. The first case reports date back to 2015. But no one wanted to hear it-because the revenue stream was too sweet.
And now we’re seeing a cascade: rapid weight loss → adipocyte lysis → increased hepatic cholesterol flux → biliary crystallization. It’s a perfect storm engineered by pharmaceutical marketing.
UDCA trials? Cute. But why not just *slow the weight loss*? That’s the real intervention. Not a drug to fix a drug. Stop the bleed before you patch the hole.
Also, ‘no fasting needed’ for ultrasound? That’s the only sane thing in this entire debacle. Why isn’t this standard of care? Because medicine still thinks ‘watchful waiting’ is a strategy. It’s not. It’s negligence dressed in white coats.
Louise Girvan
December 7, 2025 AT 03:41Obesity is a ‘disease’? Nah. It’s a symptom. The real disease? Corporate greed. They sell you a drug that breaks your body so you’ll buy the fix. Again. And again. And again.
And you? You’re still taking it. Because you trust them. 🤡
soorya Raju
December 8, 2025 AT 00:28Dennis Jesuyon Balogun
December 8, 2025 AT 14:02Let me speak to the collective trauma here. We’ve been sold a narrative: lose weight, be healthy, be worthy. But the body doesn’t care about your Instagram profile. It cares about balance.
GLP-1 agonists don’t heal-they override. They silence hunger, but they also silence your gallbladder’s voice. And when you silence a system that’s been working for 2 million years, it doesn’t just whisper back. It explodes.
For those of us in the Global South, this isn’t just a medical issue. It’s a colonial one. We’re importing Western pharmaceutical solutions to problems rooted in systemic neglect-poor food access, stress, sleep deprivation-and then blaming the body when the solution backfires.
Slow weight loss isn’t a suggestion. It’s an act of reverence. Respect your bile. Respect your organs. Respect your history.
And if you’re reading this and you’re in pain? You’re not weak. You’re not failing. You’re signaling. Listen. Then get scanned. Not because you’re broken-but because you’re human.
And if your doctor won’t order the ultrasound? Find one who will. Your life isn’t a clinical trial. It’s your only one.
Grant Hurley
December 9, 2025 AT 14:14Lucinda Bresnehan
December 10, 2025 AT 23:30I’m a nurse practitioner and I’ve seen this too many times. A 58-year-old woman comes in with right upper quadrant pain after eating fried chicken. She’s on Ozempic. She says, ‘I thought it was just heartburn.’ I order the ultrasound. Gallstones. Big ones.
She’s terrified. She says, ‘But I’m doing everything right!’
And I say: You *are* doing everything right. You’re taking care of your diabetes, losing weight, being proactive. But you weren’t warned. That’s on us.
Now I screen every woman over 40 with BMI >30 before they start. I tell them: ‘If your right rib hurts after fat, don’t wait. Get checked.’
It’s not fear. It’s care.
And yes-UDCA might help. But the real win? Slowing weight loss. It’s cheaper, safer, and your body actually adapts.
Also, if you’ve had your gallbladder removed? You’re golden. No sludge storage. No problem. But watch for jaundice. That’s the red flag for bile ducts.
Love you all. Please get checked. You deserve to be healthy without collateral damage.
Shannon Gabrielle
December 12, 2025 AT 01:30