GLP-1 Receptor Agonists: How They Help You Lose Weight and Lower A1C
For years, managing type 2 diabetes meant choosing between medications that lowered blood sugar but made you gain weight-or ones that didn’t help much with weight at all. That changed when GLP-1 receptor agonists came on the scene. These aren’t just another diabetes drug. They’re changing how doctors treat both high blood sugar and obesity at the same time. If you’ve heard about Ozempic or Wegovy in the news, you’re not alone. People are losing weight, feeling less hungry, and seeing their A1C drop-sometimes by more than 1.8%. But how do they actually work? And what’s the catch?
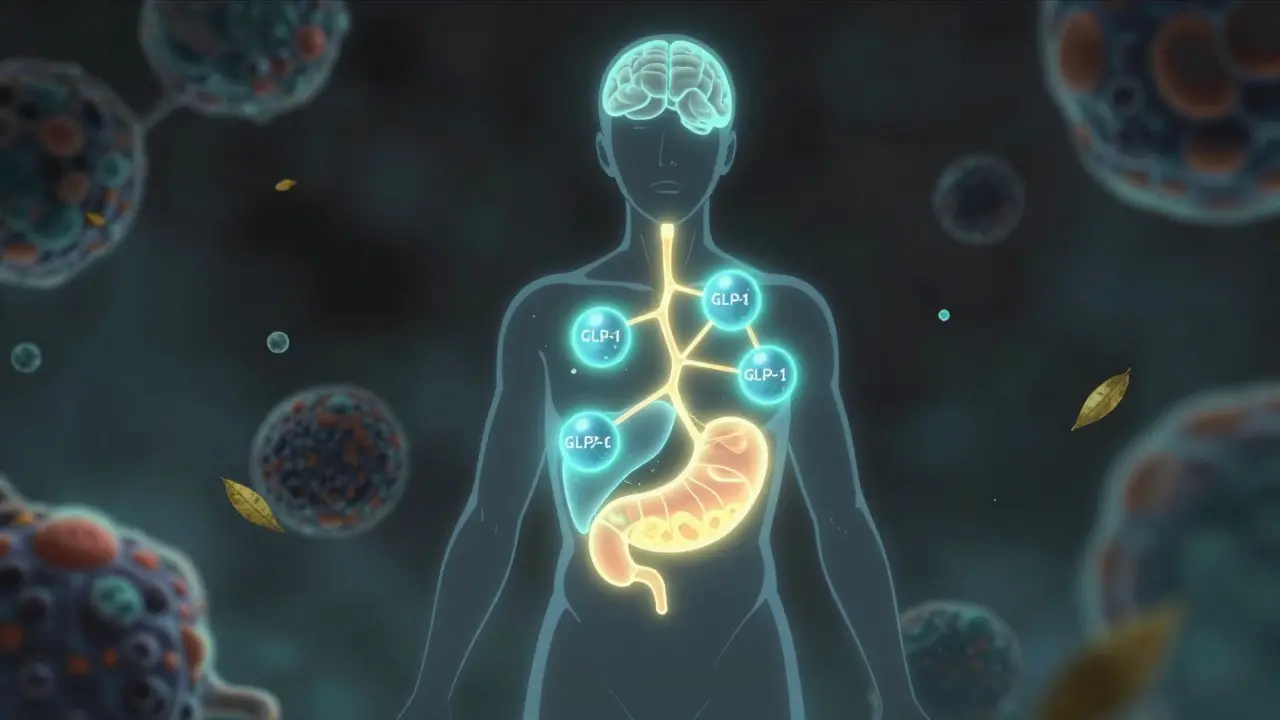
How GLP-1 Receptor Agonists Work in Your Body
GLP-1 receptor agonists mimic a natural hormone your gut makes after you eat. This hormone, called glucagon-like peptide-1, tells your body what to do next: slow down digestion, tell your pancreas to release insulin only when needed, and signal your brain that you’re full. That’s it. No magic. Just your body’s own system turned up a notch.
When you take a GLP-1 agonist like semaglutide or liraglutide, it binds to receptors in three key places: your pancreas, your stomach, and your brain. In the pancreas, it boosts insulin release when blood sugar rises-without causing dangerous lows. At the same time, it cuts down on glucagon, the hormone that tells your liver to pump out more sugar. That’s why A1C levels drop. In clinical trials, most people saw their A1C fall by 1.0% to 1.8%. For someone starting at 8.5%, that’s moving from poorly controlled to well-controlled diabetes.
But here’s the game-changer: it also slows down how fast food leaves your stomach. That’s why you don’t get those spikes in blood sugar after meals. It’s not just about insulin-it’s about timing. Slower digestion means glucose enters your bloodstream gradually, not all at once.
And then there’s your brain. GLP-1 activates areas in the hypothalamus that control hunger. It turns down the volume on signals that make you crave food, especially carbs and sweets. Studies show people on these drugs report feeling satisfied with smaller portions. One user on Reddit said, “I used to snack all day. Now I just don’t think about food like that.” It’s not willpower. It’s biology.
Weight Loss Results You Can Actually Expect
Weight loss with GLP-1 agonists isn’t small. It’s not “a few pounds.” It’s life-changing. In the STEP 3 trial, people taking semaglutide (Wegovy) lost an average of 15.3 kg-about 14.9% of their starting weight-over 68 weeks. Nearly 9 out of 10 lost at least 5% of their body weight. Almost 7 out of 10 lost 10% or more. Half lost 15% or more.
Compare that to other diabetes drugs. Sulfonylureas? They make you gain 2-4 kg. Insulin? Often 4-10 kg. Even DPP-4 inhibitors, which are oral pills, barely move the needle-maybe half a kilo either way. GLP-1 agonists are the only class that consistently helps people lose weight while improving blood sugar.
And it’s not just semaglutide. Tirzepatide (Zepbound), a newer dual agonist that also targets GIP, showed even bigger results in the SURMOUNT trials: 20.9% average weight loss at the highest dose. That’s comparable to what you’d see after gastric bypass surgery. But without the surgery.
Real-world results match clinical data. One user lost 105 pounds over 14 months on semaglutide. Another lost 18% of body weight in six months. These aren’t outliers-they’re becoming the norm for people who stick with the treatment.
Why These Drugs Are Better Than Other Diabetes Medications
Let’s say you’re on metformin. It’s good. It helps with blood sugar and might help you lose a little weight. But it doesn’t do what GLP-1 agonists do. It doesn’t slow your stomach. It doesn’t shut down cravings. It doesn’t make you feel full after a salad.
Or consider SGLT2 inhibitors like empagliflozin. They help you lose weight-about 2-5 kg-by making your kidneys dump sugar in your urine. But they don’t touch appetite. And they come with risks like yeast infections and dehydration.
GLP-1 agonists work differently. They’re not just lowering glucose-they’re resetting your metabolism. They improve insulin sensitivity, reduce liver fat, and even lower blood pressure slightly. The LEADER trial showed liraglutide reduced heart attacks, strokes, and heart-related deaths by 13% in high-risk patients. That’s why the American Diabetes Association now recommends them for people with type 2 diabetes who also have heart disease or are at high risk.
And unlike insulin, you don’t need to check your blood sugar constantly or worry about low blood sugar episodes. GLP-1 agonists are glucose-dependent. They only work when you need them. That’s a huge safety advantage.

The Catch: Side Effects and How to Handle Them
These drugs aren’t side-effect free. About 30-50% of people experience nausea, especially when starting or increasing the dose. Vomiting happens in 5-10%. Diarrhea and constipation are common too. Most of this happens in the first 4-8 weeks.
The key is slow titration. You don’t start at the full dose. For Wegovy, you begin with 0.25 mg once a week. After four weeks, you go to 0.5 mg. Then 1.0 mg, then 1.7 mg, and finally 2.4 mg. Each step takes at least a month. Rushing it makes side effects worse.
Doctors recommend taking the shot at night. That way, if you feel queasy, you’re asleep. Avoid high-fat meals during the first few weeks. Stick to lean proteins, veggies, and simple carbs. Drink plenty of water. Over-the-counter meds like dimenhydrinate (Dramamine) can help with nausea.
Needle anxiety? It’s common. But most people get used to it after 2-3 tries. The pens are small, with thin needles. Many come with hidden needles and automatic injection. Novo Nordisk reports that 85% of patients master self-injection after proper training.
And yes-weight comes back if you stop. Studies show people regain 50-70% of lost weight within a year of quitting. That’s not failure. It’s biology. These drugs don’t cure obesity-they manage it. Like blood pressure or cholesterol meds, they work while you take them.
Cost, Access, and Insurance Hurdles
Here’s the hard truth: these drugs are expensive. Without insurance, a month’s supply of Wegovy or Ozempic can cost $800-$1,200. That’s why so many people can’t get them.
In the U.S., Medicare Part D covers about 62% of prescriptions-but only if you’ve tried and failed other weight-loss methods first. Private insurers often require prior authorization, proof of obesity (BMI ≥30), and sometimes a diagnosis of prediabetes or metabolic syndrome.
Some pharmacies offer discount cards, but they rarely bring the price below $500/month. In Canada, access is better through provincial drug plans, but wait times for approval can be months long. In Halifax, many patients report delays of 3-6 months before getting coverage.
And supply shortages are real. The FDA has listed semaglutide as in shortage since early 2022. Pharmacies ration doses. Some clinics prioritize patients with diabetes over those using it for weight loss alone.

What’s Next? New Drugs and Broader Uses
The field is moving fast. Tirzepatide (Zepbound) is already approved for obesity and diabetes. It’s more effective than semaglutide in head-to-head trials. Oral versions of semaglutide are now available-no injections needed. They’re not as potent as the injectables, but they’re a big step forward for people who hate needles.
Researchers are testing these drugs for more than just weight and blood sugar. A 2024 study in The Lancet showed semaglutide reduced liver fat by over 50% in people with fatty liver disease. Another trial found it improved heart failure symptoms in obese patients. Novo Nordisk is even studying whether it can slow Alzheimer’s progression.
But long-term safety data beyond five years is still limited. The FDA and health agencies are watching closely. So far, no new major risks have popped up, but we’re still learning.
Who Should Consider These Drugs?
You might be a good candidate if:
- You have type 2 diabetes and are struggling to get your A1C under control
- You have obesity (BMI ≥30) or overweight with a weight-related condition like high blood pressure or sleep apnea
- You’ve tried diet and exercise but haven’t lost meaningful weight
- You’re willing to commit to long-term use and manage side effects
- You can access insurance coverage or afford out-of-pocket costs
You should talk to your doctor if you have a history of pancreatitis, medullary thyroid cancer, or multiple endocrine neoplasia syndrome. These drugs aren’t for everyone.
And remember-these aren’t magic pills. They work best with healthy eating, regular movement, and behavioral support. They give you a biological advantage. But you still have to show up.
Do GLP-1 agonists cure diabetes?
No. GLP-1 agonists help manage type 2 diabetes by improving blood sugar control and reducing A1C levels, but they don’t cure the disease. If you stop taking them, blood sugar levels typically rise again. They’re a long-term treatment, not a one-time fix.
Can I take GLP-1 agonists if I don’t have diabetes?
Yes. Wegovy and Zepbound are FDA-approved specifically for chronic weight management in adults with obesity or overweight and at least one weight-related condition-even if they don’t have diabetes. These drugs are being used more for weight loss than for blood sugar control in many cases.
How long does it take to see results?
Most people start noticing reduced hunger and slight weight loss within the first 2-4 weeks. But full effects on A1C and weight take time. The biggest changes usually happen after 16-20 weeks, once you reach the full maintenance dose. Clinical trials show maximum weight loss occurs around 68 weeks.
Are these drugs safe for long-term use?
Current data shows GLP-1 agonists are safe for long-term use in most people. The LEADER trial followed patients for over 5 years and found no new safety signals. However, long-term data beyond 10 years is still limited. Regular check-ups with your doctor are essential to monitor kidney function, thyroid health, and gastrointestinal symptoms.
Will insurance cover GLP-1 agonists for weight loss?
Coverage varies widely. In the U.S., Medicare and many private insurers require prior authorization and proof that you’ve tried other weight-loss methods first. Some plans only cover them for people with diabetes. In Canada, provincial drug plans may cover them, but approval can take months. Always check with your insurer before starting treatment.
What happens if I stop taking the drug?
Most people regain 50-70% of lost weight within a year of stopping. This isn’t because you failed-it’s because the drug was managing your appetite and metabolism. Without it, your body returns to its previous state. For that reason, many experts recommend continuing treatment indefinitely, similar to how people take blood pressure or cholesterol medications.
If you’re considering a GLP-1 agonist, talk to your doctor about your goals, your health history, and what you’re willing to commit to. These drugs are powerful-but they work best when you’re informed, supported, and ready for the long haul.
Shawn Raja
January 24, 2026 AT 22:32So let me get this straight-we’ve turned biology into a subscription service? You don’t cure obesity, you rent it. Like Netflix for your appetite. And if you stop paying? Your stomach throws a tantrum and your brain starts screaming for pizza. Welcome to capitalism, folks. We monetized hunger and called it medicine.
Shweta Deshpande
January 25, 2026 AT 17:47OMG I just started semaglutide last month and I’m already noticing the difference-like, I used to eat a whole bag of chips while watching Netflix at 2am, now I just… don’t even think about it? It’s wild. I’m not even trying that hard, I just feel full after a small bowl of soup. My mom says I look like a different person, and honestly? I feel like one too. My A1C dropped from 8.1 to 6.3 in three months and I’ve lost 18 lbs. It’s not magic, but it feels like it. Thank you to the scientists who made this possible 🙏
Jessica Knuteson
January 27, 2026 AT 15:29It’s not the drug that’s revolutionary it’s the fact that we’ve outsourced willpower to a pharmaceutical company
Ashley Porter
January 28, 2026 AT 16:22The pharmacokinetics here are fascinating-GLP-1 agonists exert a multimodal effect on the central appetite regulatory axis via the arcuate nucleus and NPY/AgRP neuron modulation, while simultaneously enhancing insulin sensitivity through peripheral AMPK activation. The real clinical value lies in the dissociation between glycemic control and weight gain, which is unprecedented in antidiabetic pharmacotherapy. Most agents are either weight-neutral or weight-promoting; this class flips the script entirely.
Kipper Pickens
January 30, 2026 AT 05:01Let’s not ignore the elephant in the room-these drugs are being used as aesthetic tools by people who don’t have diabetes. The market’s been hijacked by influencers selling ‘Ozempic glow’ while actual diabetics wait months for prescriptions. It’s a systemic failure. We’re treating obesity like a fashion trend, not a chronic disease. And now the supply chain’s collapsing because rich people want to look good in bikini season.
Aurelie L.
February 1, 2026 AT 03:40I tried it. Nausea for three weeks. Felt like I was dying. Gave up. Now I’m back to eating cookies. Life’s too short for injectable regret.
Joanna Domżalska
February 1, 2026 AT 20:04They say it resets your metabolism. But what if your metabolism was fine and you just ate too much? Maybe the problem isn’t biology. Maybe it’s laziness dressed up as a disease.
Sally Dalton
February 2, 2026 AT 06:52im so glad im not alone in this!! i was scared to tell anyone i was on it bc everyone was like oh u just wanna be skinny but its not that at all its like my brain finally stopped screaming for food and i can actually enjoy meals without feeling guilty?? also i cried when my dr said my a1c was 5.8 like for real tears. this drug gave me my life back and i dont care if its expensive i would pay twice as much
eric fert
February 2, 2026 AT 18:41Let’s be honest-this isn’t medicine. It’s a Band-Aid on a bullet wound. We’ve created a system where the only solution to systemic health failure is a $1,000/month injection. We don’t fix food deserts. We don’t fix stress. We don’t fix sleep. We just give people a chemical to silence their hunger while the real causes rot in the background. And then we pat ourselves on the back like we’re heroes. We’re not. We’re just really good at treating symptoms while ignoring the disease of society.
Dan Nichols
February 3, 2026 AT 16:20People don’t realize these drugs don’t make you lose weight they make you stop wanting to eat. That’s not weight loss that’s suppression. And suppression isn’t health it’s control. If you need a drug to feel full you’re not healed you’re dependent
Uche Okoro
February 4, 2026 AT 11:28The real issue isn’t the drug-it’s the commodification of metabolic dysfunction. In Nigeria, we have people dying from starvation while Americans pay $1,200/month to suppress appetite. This isn’t progress. This is pathology dressed in white coats and clinical trials. The global inequity here is obscene. We are not curing diabetes-we are monetizing desperation.
shivam utkresth
February 5, 2026 AT 22:37Bro I took tirzepatide for 6 months and lost 22kg and my A1C dropped to 5.4. But honestly? The best part wasn’t the weight loss-it was that I stopped feeling ashamed every time I walked into a restaurant. I used to order salad just to look healthy. Now I eat steak and feel full. My mom cried when she saw me. This isn’t magic. It’s dignity.
SWAPNIL SIDAM
February 7, 2026 AT 22:09My cousin lost 100 pounds on Ozempic. Now she’s happy. She got engaged. She runs marathons. I’m jealous. I can’t afford it. But I’m happy for her. She deserves it.
Geoff Miskinis
February 8, 2026 AT 15:36Interesting how the same people who decry Big Pharma now worship these drugs like holy water. The irony is thick enough to spread on toast. You want a cure? Then fix the food system. Stop blaming biology. Stop glorifying injections. This isn’t science-it’s spiritual bypassing with a syringe.