How to Verify Dose Changes and Avoid Miscommunication in Healthcare

Why Dose Verification Matters More Than Ever
Every year, thousands of patients in the U.S. are harmed because someone gave them the wrong dose of medicine. Not because the doctor made a mistake on paper, but because the message got lost in translation-between shifts, between systems, between people. A nurse reads "10U" on a prescription and assumes it means ten units. The doctor meant 1.0 unit. The patient gets ten times the insulin they should. That’s not rare. It’s predictable. And it’s preventable.
The problem isn’t just human error. It’s how we’ve designed the system. We’ve asked nurses and pharmacists to do more with less, then told them to double-check everything. But when you’re running between five rooms during a 12-hour shift, "double-check" becomes a checkbox, not a safety net. Studies show that when verification feels like busywork, people skip it. And when they skip it, mistakes happen.
The Three-Step Verification Process That Actually Works
There’s no magic bullet. But there is a proven method: the three-step verification process endorsed by the Institute for Safe Medication Practices (ISMP). It’s not about doing more. It’s about doing the right things at the right time.
- Independent calculation - Two qualified staff members calculate the dose separately, without talking to each other. For insulin, heparin, or opioids, this isn’t optional. It takes 2-3 minutes. That’s the cost of safety.
- Context check - Does this dose make sense for this patient? Is their kidney function stable? Are they on other drugs that interact? Is this a pediatric patient? Weight-based dosing must be precise to 0.1 mg/kg. A 5-year-old isn’t a small adult. This step adds 1-2 minutes but catches 70% of errors that calculators miss.
- Bedside verification - Scan the patient’s wristband. Scan the medication. Confirm the system says "match." This isn’t about technology replacing people-it’s about technology catching what people might miss. Barcode systems prevent 86% of wrong-drug or wrong-dose errors, but only if they’re used correctly. And they’re only effective if scanning compliance hits 95% or higher.
This isn’t theory. At Johns Hopkins Hospital, teams that followed this exact sequence reduced dose verification errors by 37% in 2022. The key? They didn’t add time-they protected it. Nurses got 15-20 minutes per shift labeled "safety time." No interruptions. No distractions. Just verification.
When Double Checks Fail (And What to Do Instead)
Independent double checks sound perfect. Two people look at it. Twice as safe, right? Not always.
Studies show that when double checks are used everywhere-on every pill, every IV bag, every oral dose-they become meaningless. Nurses start looking at each other’s work instead of doing their own. They nod along. They assume the other person saw it. That’s called "complacency through repetition." Dr. Michael Cohen of ISMP calls it the "illusion of safety."
Here’s the truth: you don’t need to double-check everything. You need to double-check what matters most.
Target high-alert medications: insulin, heparin, opioids, chemotherapy agents, IV potassium, and warfarin. These are the drugs that kill if dosed wrong. In 2023, ISMP identified 19 high-alert medications that require extra verification. That’s it. Not 190. Not 1,900.
For everything else? Use technology. Smart infusion pumps with dose-error reduction software catch 85% of overdose errors. But they can’t catch the wrong patient. That’s still on you. So use barcode scanning for patient ID, and save the human double check for the high-risk stuff.
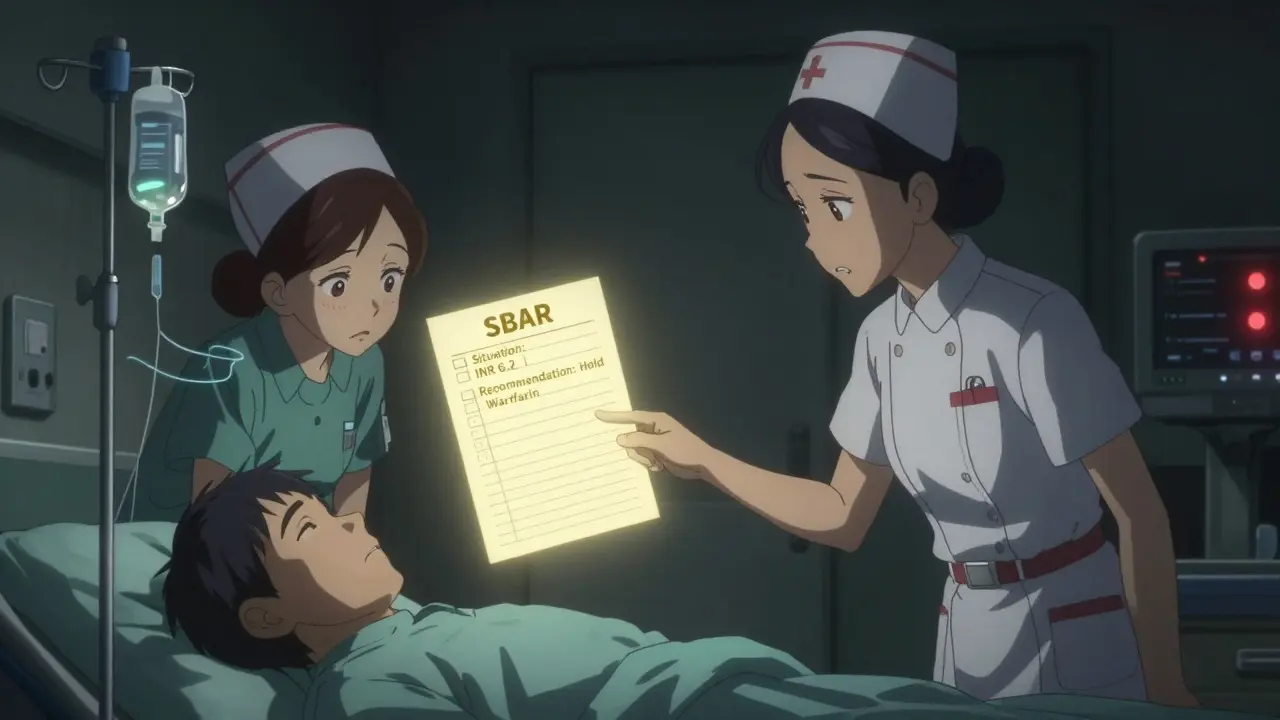
How Miscommunication Kills: The SBAR Fix
Most dose errors happen during handoffs. Shift changes. Transfers from ER to floor. Discharges. That’s when information gets chopped, rushed, or lost.
A 2020 study by Duke University found that using SBAR-Situation, Background, Assessment, Recommendation-cut miscommunication-related errors by 41%. Here’s how it works:
- Situation: "I’m calling about Mr. Johnson in Room 304. His INR jumped to 6.2 this morning."
- Background: "He’s on warfarin for atrial fibrillation. Started 3 mg last week. No new meds or diet changes."
- Assessment: "His bleeding risk is high. He’s at risk for GI bleed."
- Recommendation: "I recommend holding warfarin today and repeating INR in 24 hours."
This isn’t bureaucracy. It’s clarity. It’s the difference between a nurse hearing "change his warfarin" and knowing exactly what to change, why, and when.
When you skip SBAR, you’re gambling. A nurse on AllNurses.com shared a near-miss: "I almost gave 10 units of insulin because the order said '10U'-the doctor meant '1.0U.' The double check caught it. But if I’d just been told, 'reduce his insulin,' I’d have missed it."
Technology Isn’t the Answer-Unless It’s Used Right
Barcode systems. Smart pumps. AI alerts. These tools are powerful. But they’re not foolproof.
BCMA systems prevent 86% of wrong-drug errors. But if the barcode is smeared, or the nurse scans the wrong bag, it won’t help. One pharmacist reported a 10-fold dosing error that the system didn’t catch because the concentration was entered correctly-even though the dose was ten times too high. The machine didn’t know the dose was wrong. Only the human did.
Smart pumps reduce overdose errors by 85%. But they can’t detect if the wrong patient is in the bed. Or if the IV line is mislabeled. Or if the drug was drawn up wrong in the pharmacy.
AI tools like Epic’s DoseRange Advisor now flag unusual doses before they’re even ordered. In a 12-hospital trial, it cut inappropriate dose changes by 52%. That’s huge. But AI can’t replace context. It can’t know that a patient just had dialysis and needs a lower dose. That’s still on you.
Technology is a tool. Not a replacement. Use it to catch the easy mistakes. Save your brainpower for the hard ones.
What Happens When Verification Breaks Down
The numbers don’t lie. In 2022, ECRI Institute recorded 1,247 reported incidents of inadequate dose verification. 287 of them caused patient harm. 18 resulted in death.
Why? Three big reasons:
- Workload overload: Nurses skip steps when they’re behind. A 2022 ANA survey found 73% of nurses admitted skipping verification during peak hours. Errors jumped 22% on 12-hour shifts.
- Alert fatigue: Nurses get 15-20 alerts per shift from barcode systems. Most are false alarms. After a while, they stop paying attention. One nurse said, "I’ve learned to ignore the beeps."
- Shift handoffs: 61% of verification failures happen between 6-8 AM and 6-8 PM. That’s when people are tired, rushed, and distracted.
And here’s the worst part: incomplete documentation. AHRQ found that 29% of verification failures happened because someone didn’t write down who checked what, when. If no one records it, it didn’t happen. And if it didn’t happen, no one knows it was missed.

How to Build a Culture of Safety-Not Just Compliance
Regulations are changing. The Joint Commission now requires "reliable processes" for verifying high-risk dose changes under NPSG.01.01.01, effective January 1, 2024. CMS will penalize hospitals with over 0.5% dose verification error rates.
But rules alone won’t fix this. You need culture.
At Johns Hopkins, they didn’t just train nurses. They changed the conversation. Instead of saying, "Did you double-check?" they started asking, "Did you feel safe giving this dose?"
They created "safety pauses"-moments during the shift where anyone could stop and say, "Wait. Something doesn’t feel right." No blame. No punishment. Just time to think.
They trained staff using simulation, not PowerPoint. Real-life scenarios. High-pressure situations. The kind of thing that happens when you’re short-staffed and the IV pump alarms for the third time.
And they tracked not just compliance-but confidence. Nurses who felt supported were 43% more likely to speak up when something felt off.
What You Can Do Today
You don’t need a hospital-wide overhaul to make a difference. Start here:
- Identify your high-alert meds. Insulin. Heparin. Opioids. Potassium. Warfarin. Know them. Know the doses. Know the risks.
- Use SBAR during handoffs. Even if it’s just a quick text: "Patient X, INR 6.2, holding warfarin, repeat in 24."
- Protect your verification time. Block 15 minutes in your shift. No interruptions. Just verification.
- Scan every time. Even if it’s annoying. Even if it’s slow. Even if you’ve done it a hundred times.
- Speak up. If a dose feels wrong-even if you’re not sure-say something. You’re not being difficult. You’re being the safety net.
Medication safety isn’t about perfection. It’s about layers. One person might miss it. Two might miss it. But if you’ve got calculation, context, scanning, communication, and courage? That’s how you stop the error before it reaches the patient.
What’s Next for Dose Verification
The future is here-and it’s quieter than you think.
Voice recognition tools are being tested at Mayo Clinic. Nurses say their documentation time dropped 65%. No typing. No clicking. Just say: "Verified insulin dose for patient 304. Double-checked with nurse Smith. INR stable."
Blockchain systems are being piloted to create unchangeable logs of every dose change. Who ordered it? Who verified it? When? Where? It’s not sci-fi. It’s coming.
But the biggest shift? From universal double checks to targeted verification. You don’t need to check everything. You need to check what matters. That’s the future. And it’s already saving lives.

Alex LaVey
February 3, 2026 AT 19:41Love this breakdown. The three-step process is simple but powerful-especially the context check. Too many systems treat verification like a checklist, not a thinking exercise. Real safety isn’t about doing more-it’s about doing the right things with your brain fully engaged.
Joseph Cooksey
February 3, 2026 AT 21:23Let me be blunt: we’ve turned patient safety into a performance art. Nurses are expected to be pharmacists, data-entry clerks, and emotional support animals-all while being scolded for not following protocol. The ‘safety time’ initiative at Johns Hopkins? That’s the only thing that actually works. You can’t fix human error by adding more steps-you fix it by giving humans space to breathe. And yet, administrators still think slapping on another barcode scanner will solve everything. It won’t. It just adds another beep to the noise.
And don’t get me started on ‘alert fatigue.’ If your system is screaming at you 15 times a shift and 14 of them are false, you’re not training people to be careful-you’re training them to ignore the system. That’s not safety. That’s suicide by automation.
The SBAR method? Brilliant. But only if people actually use it. Right now, it’s just another bullet point in the orientation packet. No one’s held accountable for skipping it. No one’s rewarded for doing it well. Until we stop treating communication like a compliance checkbox and start treating it like a lifeline, we’re just rearranging deck chairs on the Titanic.
And AI? Don’t get me started. AI can flag a weird dose, but it can’t tell you that Mrs. Rivera skipped breakfast, has renal impairment, and is terrified of needles. That’s why we still need humans. Not to scan barcodes. Not to double-check numbers. But to listen. To think. To care.
We’re not failing because we’re lazy. We’re failing because we’ve built a system that punishes care.
Meenal Khurana
February 5, 2026 AT 09:10SBAR works. Simple. Clear. Done.
Joy Johnston
February 6, 2026 AT 23:14As a nurse for 18 years, I’ve seen every version of this play out. The most dangerous myth? That ‘double-checking’ is the solution. I’ve watched two nurses nod at each other and move on-neither actually looked at the label. The real game-changer? When we started asking, ‘Does this feel right?’ Not ‘Did you check it?’ but ‘Do you feel safe giving it?’ That shift-from compliance to confidence-changed everything. We stopped rushing. We started talking. And the errors? They dropped. Not because we added tech. Because we trusted each other.
Also-scan every time. Even if it’s 2 a.m. and you’re on your fifth IV. Even if you’ve done it a hundred times. The machine doesn’t care if you’re tired. But the patient does.
And yes-block your safety time. No exceptions. If someone interrupts, say, ‘I’m in safety mode. I’ll be right with you in two minutes.’ They’ll learn. Or they won’t. But you’ll still be alive tomorrow.
Lorena Druetta
February 7, 2026 AT 01:01This post made me cry. Not because it’s sad-but because it’s true. I work in a rural ER. We’re short-staffed, underfunded, and expected to be perfect. I’ve had nights where I had to choose between checking a dose and helping a patient who was choking. That’s not a choice any nurse should have to make. But we make it every day.
The ‘safety pause’ idea? That’s the first thing I’ve heard in years that gives me hope. Not because it’s fancy. Because it’s human. If we could just have one moment-just one-where we’re allowed to say, ‘Wait, something’s off,’ without being called a complainer… we’d save lives. Not with more tech. With more courage.
Thank you for writing this. I’m printing it out and putting it on the med cart.
Justin Fauth
February 7, 2026 AT 22:20Look, I don’t care what your ‘proven method’ is. If you’re in the U.S. healthcare system, you’re already behind. We’ve got nurses working 16-hour shifts because hospitals are cutting costs to boost profits. You think they care about SBAR? They care about not getting fired for being late to lunch. This isn’t a safety problem-it’s a capitalism problem. You can’t fix systemic neglect with checklists. You need to fix the system. Or stop pretending you care.
Amit Jain
February 8, 2026 AT 07:59From India, we don’t have barcode scanners or smart pumps. But we use SBAR. We write everything down. We double-check insulin doses with two nurses, even if we’re tired. Because if we don’t, someone dies. Simple. No tech needed. Just discipline. And respect for the job.
Daz Leonheart
February 8, 2026 AT 14:21Just wanted to say thank you. I’m a new nurse. This post is the first thing that didn’t make me feel like I’m failing. I’ve been scared to speak up-thought I’d sound dumb. But if even one person says ‘something feels off’ and we stop? That’s enough. I’m starting my safety pause tomorrow. No one’s gonna stop me.
Janice Williams
February 9, 2026 AT 20:12While the three-step verification process sounds theoretically sound, it ignores the fundamental reality of healthcare economics. Institutions prioritize efficiency over safety because safety is expensive. The ‘15-minute safety window’ is a luxury most hospitals cannot afford. This is not a clinical problem-it is a financial one. Until hospitals are financially incentivized to reduce errors-not penalized for them-this entire framework is a performative gesture. The real solution? Nationalize healthcare. Then we can talk about safety.
Coy Huffman
February 10, 2026 AT 05:46It’s funny how we treat medicine like a machine, but the only thing that saves lives is the human moment-the pause, the question, the hesitation before pressing ‘confirm.’ We’ve outsourced our conscience to algorithms and checklists, then wonder why people stop caring. Maybe safety isn’t about protocols. Maybe it’s about remembering that behind every dose is a person who trusts you not to mess up. And that’s not something you can scan.
Shelby Price
February 10, 2026 AT 10:13So… we’re saying the answer is to slow down? 😅