Immunocompromised Patients and Medication Reactions: Special Risks
Immunocompromised Medication Risk Calculator
Select Your Medications
>20mg prednisone equivalent: 60% higher infection risk
70% effectiveness but 50% stop within 1 year due to side effects
Risk of Pneumocystis pneumonia and tuberculosis reactivation
Higher infection risk than traditional drugs; common shingles reactivation
Virus reactivation risks (EBV, Hepatitis B)
Risk increases by over 200% compared to single drug
Risk Assessment Results
Key Risks
Selected medications:
Critical Safety Information
Remember:
- Atypical Symptoms: Infections often lack fever or redness due to suppressed immune response.
- Vaccines: Only inactivated vaccines (flu shot, pneumonia shot) are safe. Avoid live vaccines.
- Monitoring: Monthly blood tests are essential for early detection of complications.
- Immediate Action: If you feel "off" (fatigue, confusion, achiness), contact your doctor immediately.
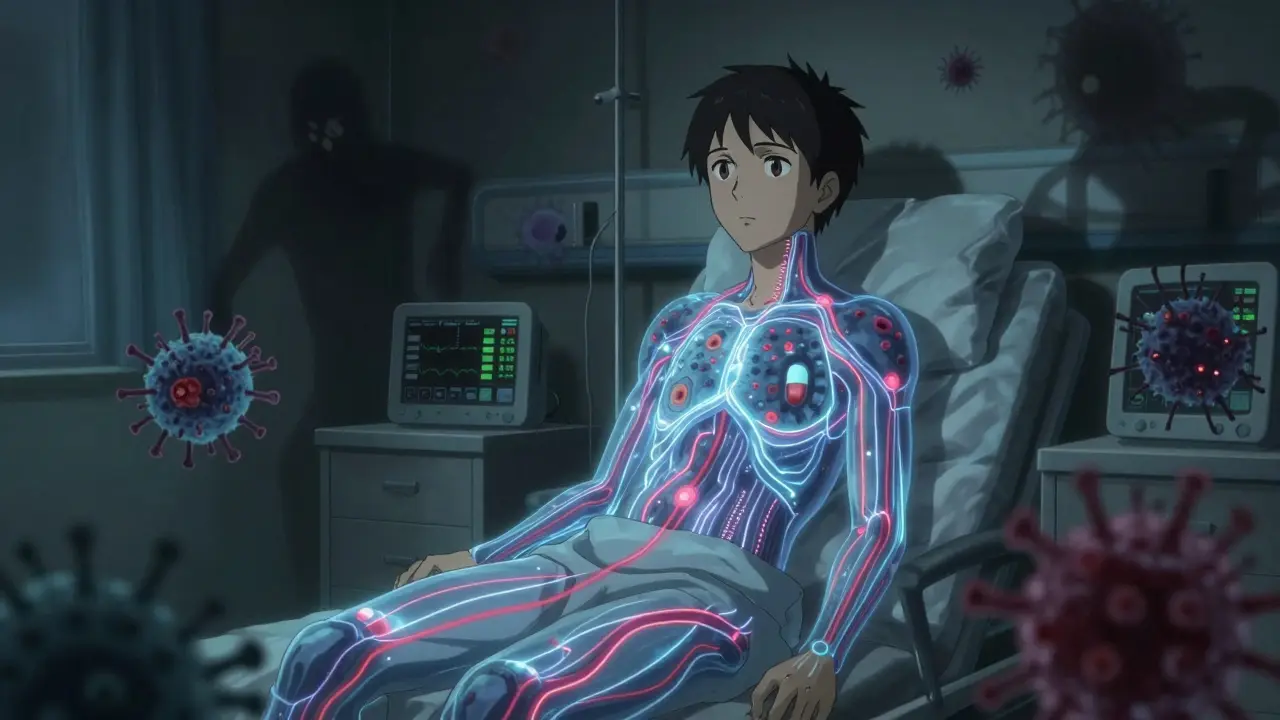
When your immune system is already struggling, taking medication can become a high-stakes game. For immunocompromised patients, common drugs meant to treat autoimmune diseases or prevent organ rejection don’t just help-they can also put you at serious risk. It’s not about avoiding treatment. It’s about understanding exactly how these medications change your body’s defenses-and what that means when you get sick.
What Does "Immunocompromised" Really Mean?
Being immunocompromised isn’t a single condition. It’s a state. Your immune system isn’t working the way it should. You might not get a fever when you have an infection. You might not feel sick until it’s too late. This happens because of disease-like HIV, lupus, or leukemia-or because of the very drugs meant to control those conditions. Think of your immune system like a security team. In a healthy person, it spots trouble fast and reacts hard. In someone on immunosuppressants, that team is understaffed, confused, or even on vacation. A simple cold can turn into pneumonia. A small cut can get infected. And sometimes, you won’t even know something’s wrong until it’s serious.The Big Players: How Common Medications Work (and What They Do to You)
Not all immunosuppressants are the same. Each class attacks the immune system differently, and each brings its own set of risks. Corticosteroids like prednisone are everywhere. They’re used for asthma flares, allergic reactions, and autoimmune flare-ups. But they don’t just calm inflammation-they shut down whole parts of your immune response. At doses over 20 mg a day (prednisone equivalent), your risk of infection jumps. A 2012 study of over 4,000 patients showed steroid users had a 60% higher chance of getting infected than those on placebo. And here’s the scary part: steroids can hide the signs of infection. No fever? No redness? That doesn’t mean you’re fine. It might mean your body can’t fight back at all. Methotrexate is the most common drug for rheumatoid arthritis and psoriasis. About 70% of people find it effective. But nearly half stop taking it within a year because of side effects: fatigue, nausea, mouth sores, liver stress. Monthly blood tests are non-negotiable. Liver enzymes and white blood cell counts can crash without warning. One patient in Halifax told their rheumatologist they felt "just tired"-turns out their white blood cell count was below 1,000. They ended up in the ER with pneumonia. Azathioprine (Imuran) cuts down on T and B cells. That’s good for stopping autoimmune attacks. But it also leaves you open to bacteria, viruses, and even rare fungi. People on azathioprine have developed Pneumocystis pneumonia, tuberculosis reactivation, and progressive multifocal leukoencephalopathy (PML)-a rare, deadly brain infection caused by the JC virus. It’s rare, but when it happens, it’s often too late. Biologics like Humira, Enbrel, and Remicade are targeted. They block specific parts of the immune system, like TNF-alpha. That sounds smart. But they’re also the most dangerous when it comes to infection. Studies show biologics carry a higher infection risk than traditional drugs like methotrexate. Herpes zoster (shingles) is common. So is tuberculosis. One Reddit user in r/RheumatoidArthritis shared they got shingles three times in two years while on a TNF inhibitor. "The first time, I thought it was a bug bite. The third time, I had to be hospitalized. No one warned me how easily it could come back." Calcineurin inhibitors like cyclosporine and tacrolimus are life-saving after transplants. But they’re notorious for reactivating viruses. Epstein-Barr virus can lead to lymphoma. Hepatitis B can flare up. Polyomavirus can damage kidneys. These drugs don’t just suppress-they create blind spots in your immune system.Combination Therapy: When Risks Multiply
Many patients take more than one immunosuppressant. Steroid + methotrexate. Biologic + azathioprine. It’s common. But it’s not safe. The risk isn’t just added. It’s multiplied. A 2021 review in the Journal of Clinical Immunology found that combining steroids with another immunosuppressant raised the risk of serious infections by over 200% compared to single-drug therapy. One patient in a Halifax clinic developed invasive aspergillosis-a fungal lung infection-after being on prednisone and mycophenolate for lupus. They didn’t have a fever. They didn’t cough. They just got progressively weaker. By the time they were diagnosed, the infection had spread to their brain.
What You Can’t See: Atypical Infections
In healthy people, infections show up with clear signs: fever, chills, swelling, pain. For immunocompromised patients, those signs often vanish. A UTI might just mean confusion in an older adult. Pneumonia might look like fatigue. A skin infection might look like a rash. Doctors call this "masking." Corticosteroids blunt the body’s natural alarm system. That’s why the CDC and Cleveland Clinic both stress: if you’re immunocompromised and feel "off," even a little, get checked. Don’t wait. This is why routine monitoring matters. Monthly CBCs. Liver and kidney function tests. Regular skin checks. Even if you feel fine. One study found that 40% of immunocompromised patients with bacterial infections had normal temperatures. They didn’t know they were sick until their organs started failing.Vaccines: Help or Hazard?
Vaccines are tricky. Some are lifesavers. Others are dangerous. Live vaccines-like MMR, varicella (chickenpox), and the nasal flu spray-are off-limits. They contain weakened viruses that your immune system can’t handle. One patient in Toronto got shingles from the chickenpox vaccine because they weren’t told it was unsafe. Inactivated vaccines-flu shot, pneumonia shot, COVID-19 shot-are generally safe. But they don’t always work. Studies show immunocompromised patients often don’t build strong immunity from vaccines. That’s why extra doses are now recommended. The CDC advises three doses of the COVID-19 vaccine for most immunocompromised people, not two. And even then, protection might be partial.
Real-Life Risks: Beyond the Lab
It’s not just drugs. Your environment matters. The CDC warns that immunocompromised people are more likely to get sick from mosquitoes and ticks. Lyme disease, West Nile virus, and tick-borne encephalitis can be far more severe. Gardening, hiking, or even walking the dog in spring can carry hidden dangers. Handwashing isn’t optional. It’s survival. Wash for 20 seconds-long enough to sing "Happy Birthday" twice. Use sanitizer when soap isn’t around. Avoid crowds during flu season. Wear a mask. These aren’t "precautions." They’re your new daily routine. And yes, some people do fine. Johns Hopkins researchers found in 2021 that immunocompromised patients on biologics had similar COVID-19 outcomes as healthy people. That surprised everyone. But it doesn’t mean the risk is gone. It just means your body’s response isn’t always predictable.What You Need to Do Now
If you’re immunocompromised, here’s what actually works:- Know your meds. Ask your doctor: "What does this drug do to my immune system? What infections should I watch for?"
- Get tested regularly. Blood work isn’t optional. It’s your early warning system.
- Get the right vaccines. No live vaccines. Get extra doses of flu and COVID shots. Ask about pneumococcal and hepatitis B vaccines.
- Watch for "off" feelings. If you’re tired, achy, or just not yourself-call your doctor. Don’t wait for a fever.
- Protect yourself daily. Handwashing, masks, avoiding sick people, and clean wound care aren’t suggestions. They’re your armor.
There’s no perfect solution. Every drug has trade-offs. But knowledge turns fear into control. You don’t have to live in fear. You just have to be informed.
Can I still get vaccinated if I’m on immunosuppressants?
Yes-but only certain vaccines. Live vaccines like MMR, varicella, and the nasal flu spray are dangerous and should be avoided. Inactivated vaccines like the flu shot, pneumonia shot, and COVID-19 vaccines are safe and recommended. However, your immune system may not respond as strongly, so extra doses are often needed. Always check with your doctor before getting any shot.
Do immunosuppressants make you more likely to get cancer?
Yes, some do. Long-term use of drugs like azathioprine, cyclosporine, and certain biologics increases the risk of skin cancer and lymphoma. This is why regular skin checks and avoiding excessive sun exposure are critical. The FDA requires black box warnings on many of these drugs for this very reason. Monitoring isn’t just about infection-it’s about catching cancer early.
Why don’t I get a fever when I’m sick?
Corticosteroids and other immunosuppressants suppress the body’s ability to raise its temperature as a defense. Fever is a signal-your body’s way of telling you something’s wrong. When that signal is turned off, infections can grow unnoticed. That’s why symptoms like fatigue, confusion, chills, or a general "off" feeling are more important than fever in immunocompromised patients.
Can I travel if I’m immunocompromised?
Yes-but plan carefully. Avoid areas with high risks of vector-borne diseases like malaria or dengue. Skip destinations with poor sanitation. Get travel vaccines approved for immunocompromised patients. Carry a letter from your doctor explaining your condition. Always have access to clean water and medical care. Many hospitals now have travel clinics specifically for immunocompromised travelers.
Is it safe to be around pets if I’m immunocompromised?
Generally, yes-but with limits. Avoid reptiles, birds, and young animals-they carry higher risks of salmonella, psittacosis, and toxoplasmosis. Clean litter boxes daily (wear gloves). Don’t let pets lick your face. Wash your hands after petting. Most healthy dogs and cats are fine, but always check with your doctor if you’re on strong immunosuppressants.