Medication Safety Statistics: What Patients Need to Know to Avoid Harm

Every year, medication safety failures hurt more than 1.5 million people in the U.S. alone. That’s not a rare accident. It’s a systemic problem that touches nearly every household. You might think taking your pills exactly as prescribed is enough to stay safe. But the truth is, even perfect patients get caught in gaps no one talks about. The numbers don’t lie: 1 in 20 people globally suffer preventable harm from their medications. And it’s not just about mistakes at the pharmacy. It’s about confusion at home, dangerous drug interactions, fake pills online, and instructions that don’t make sense. This isn’t fear-mongering. It’s facts. And you need to know them.
How Common Are Medication Errors?
Medication errors aren’t rare glitches. They’re the most frequent type of medical mistake in hospitals. In the U.S., about 1.3 million people are harmed by medications each year. That’s more than car accidents or falls. And it’s not just hospitals. At home, between 2% and 33% of patients make mistakes with their prescriptions - mixing up doses, skipping pills, or taking them at the wrong time. Older adults are especially at risk. One in five seniors are prescribed antipsychotics they don’t need, and those drugs can cause falls, confusion, and even death.
IV medications are the most dangerous. In hospitals and nursing homes, nearly half of all medication errors happen with drugs given through an IV. Antibiotics, heart meds, and painkillers like opioids are the top culprits. Fentanyl-laced counterfeit pills are now the leading cause of death for Americans between 18 and 45. In 2023, the DEA seized over 80 million of these fake pills. Many were sold on social media or disguised as legitimate prescriptions.
Who’s Most at Risk?
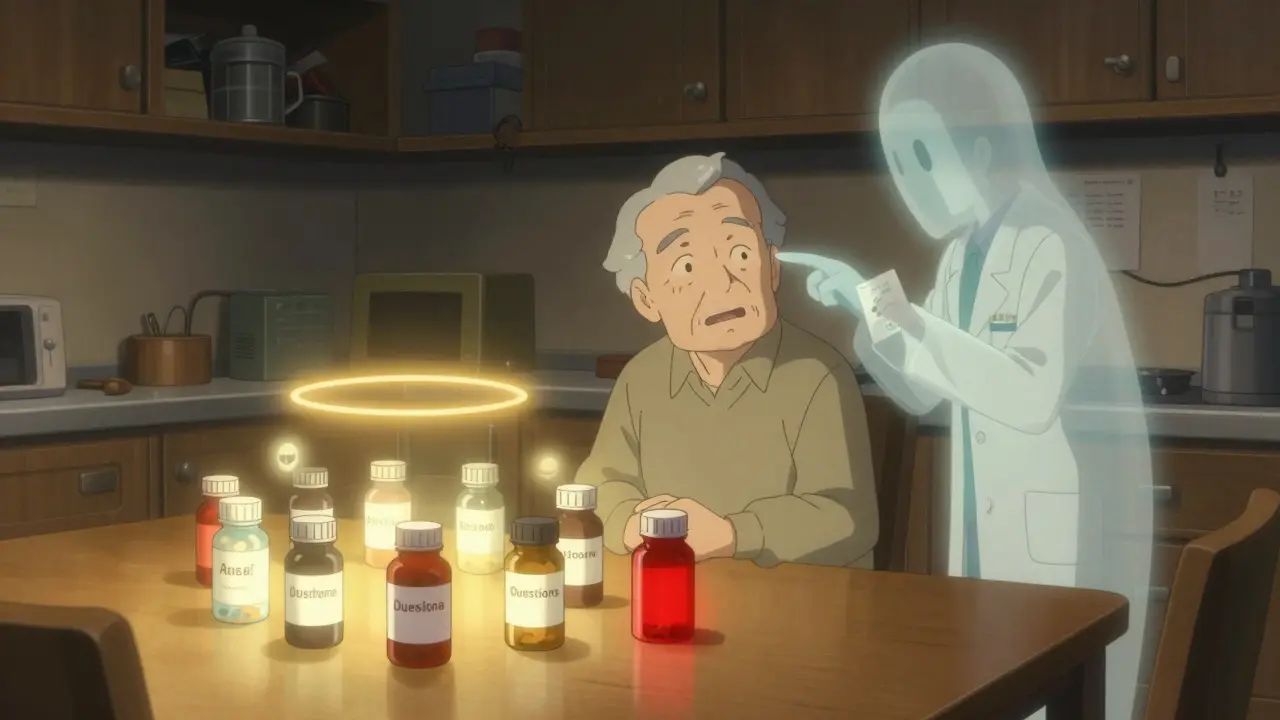
If you’re over 65, take five or more medications, or have trouble reading labels, you’re in a high-risk group. Seniors are twice as likely to be hospitalized because of a bad reaction to a drug. Why? Because their bodies process medicine differently. They’re often on multiple prescriptions from different doctors who don’t talk to each other. A 78-year-old might be taking a blood thinner, a diabetes pill, an antidepressant, a painkiller, and a statin - all with different timing, food rules, and side effects. One wrong interaction can send them to the ER.
Younger people aren’t safe either. Nearly 9 million Americans misused prescription painkillers in 2021. About 4 million misused stimulants like Adderall. Many get these drugs from friends, family, or unregulated websites. Fake oxycodone pills now make up more than half of all overdose deaths between 2019 and 2021. The DEA found that 32% of all counterfeit drug seizures happen in North America. That means if you buy pills online - even if they look real - you’re playing Russian roulette.
What’s Really Going Wrong?
Most people blame doctors or pharmacists. But experts say it’s not about who made the mistake. It’s about the system. Dr. Donald Berwick, former head of Medicare, put it simply: “Most medication errors are system failures, not individual failures.”
Here’s how the system breaks down:
- Communication gaps: Your primary care doctor doesn’t know what your cardiologist prescribed. Your pharmacist doesn’t know about the herbal supplement you’re taking.
- Poor labeling: Small print, confusing symbols, unclear instructions. One Reddit thread with over 1,200 posts found that 68% of users were confused about dosage. “Take one by mouth twice daily” sounds simple - until you realize the bottle says “take every 12 hours.”
- Technology failures: Electronic prescriptions get misread. Infusion pumps malfunction. Between January 2023 and August 2024, over 200,000 pump-related events were reported to the FDA - including 204 deaths.
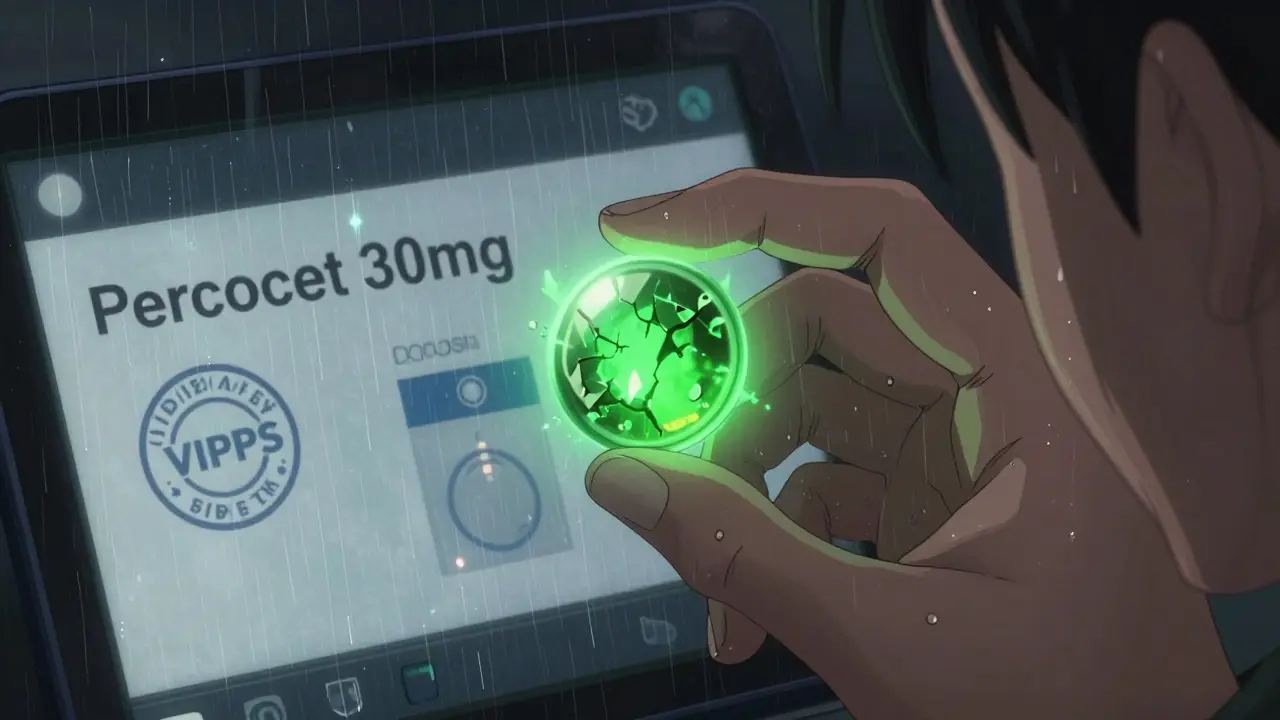
- Access to fake drugs: Online pharmacies sell counterfeit pills with no oversight. Fentanyl, rat poison, and other deadly substances are mixed into pills that look like Xanax or Percocet.
What Are the Real Costs?
The human cost is obvious: hospitalizations, ER visits, lost time at work, and death. But the financial cost is staggering. Medication errors cost the global healthcare system $42 billion every year. That’s nearly 1% of all health spending. In the U.S., adverse drug events send more than 1.5 million people to the emergency room annually. That’s one every 22 seconds.
And it’s getting worse. The global market for patient safety tools is projected to hit $14.3 billion by 2029. Why? Because hospitals, insurers, and governments are finally waking up. Medicare is now tracking 16 specific safety metrics for 2025 - including how often people take their cholesterol meds, whether they’re on too many opioids, and if dementia patients are being given dangerous antipsychotics.
What Can You Do to Protect Yourself?
You can’t control the system. But you can control your own actions. Here’s what actually works:
- Keep a living medication list. Write down every pill, patch, injection, vitamin, and supplement you take - including the dose and why you take it. Update it every time your doctor changes something. Bring this list to every appointment.
- Use one pharmacy. A single pharmacy can spot dangerous interactions. If you switch between pharmacies, they won’t see your full history.
- Ask the five questions before taking any new drug: What is this for? How do I take it? What side effects should I watch for? What happens if I miss a dose? Is there a cheaper or safer alternative?
- Check your pills. If your new prescription looks different from last time - different color, shape, or markings - ask the pharmacist. Counterfeit pills often look identical to real ones.
- Avoid online pharmacies unless they’re verified. Look for the VIPPS seal (Verified Internet Pharmacy Practice Sites). If it’s a website you found on Instagram or TikTok, don’t buy from it.
Australia’s “5 Moments for Medication Safety” approach is simple and powerful: review your meds when you start a new treatment, add a new drug, move between care settings, handle high-risk medications, and do a full review every 6-12 months. You don’t need a degree to do this. You just need to be curious.
What’s Being Done - And What’s Not Working
Some places are making progress. Australia cut opioid-related deaths by 37% since 2018 by using real-time prescription monitoring. They also reduced inappropriate antipsychotic use in seniors by 11%. The U.S. has the REMS program for high-risk drugs and the FDA’s crackdown on fake meds. The EU requires safety features on all prescription packaging.
But big gaps remain. Most hospitals still don’t use AI tools that could reduce errors by 30%. Many doctors still handwrite prescriptions. Patients are rarely trained to be active partners in their own safety. And the fake drug trade? It’s growing faster than law enforcement can stop it. Fentanyl is now easier to buy online than a new pair of sneakers.
Technology isn’t the answer unless it’s used correctly. A smart pill dispenser won’t help if you don’t understand why you’re taking the pill. A digital record won’t prevent harm if your doctors don’t talk to each other.
What You Should Do Today
Don’t wait for the system to fix itself. Start now.
- Grab your current meds and write them down. Include dosages and times.
- Call your pharmacy and ask if they have a complete list of everything you’ve picked up in the last year.
- Next time your doctor prescribes something, say: “Can you explain this to me like I’m 12?”
- Throw away any old pills you haven’t taken in six months. Don’t keep them in your bathroom cabinet.
- Block access to unverified online pharmacies on your devices.
Medication safety isn’t about being perfect. It’s about being aware. It’s about asking questions. It’s about not assuming someone else is watching out for you. The data shows that harm is preventable - but only if you take charge.
How common are medication errors in the U.S.?
About 1.3 million Americans experience medication-related harm each year, with over 1.5 million emergency room visits caused by adverse drug events. Medication errors are the most common type of medical mistake in hospitals, and at least 7,000 deaths occur annually in hospitals alone due to these errors.
What types of medications cause the most harm?
Antibiotics cause the highest share of medication-related harm at around 20%, followed by antipsychotics (19%), central nervous system drugs (16%), and cardiovascular medications (15%). IV medications have the highest error rate in hospitals - between 48% and 53%. Fentanyl-laced counterfeit pills are now the leading cause of death for Americans aged 18 to 45.
Are online pharmacies safe?
Most are not. Over 32% of counterfeit drug seizures in the world happen in North America. Fake pills sold online often contain lethal doses of fentanyl, rat poison, or other toxins. Only buy from websites with the VIPPS seal. If you found the site on social media, it’s not safe.
What should I do if my pill looks different?
Don’t take it. Call your pharmacy immediately. Counterfeit medications are designed to look identical to real ones, but small differences in color, shape, or markings can signal a fake. Pharmacists are trained to verify authenticity - use them as your first line of defense.
How can I reduce my risk of a medication error at home?
Keep an updated list of all your medications and bring it to every appointment. Use one pharmacy for all your prescriptions. Ask your doctor or pharmacist to explain each new drug in simple terms. Never skip doses or double up unless instructed. And never take pills from unlabeled containers or leftovers from old prescriptions.

Kristen Russell
January 2, 2026 AT 09:07This post hit me right in the gut. I almost lost my mom last year because a pharmacist mixed up her blood pressure meds. She didn’t even notice until her legs swelled up like balloons. Don’t wait for a crisis to get serious about your meds.
Keep a list. Use one pharmacy. Ask questions. It’s not hard. It’s just necessary.
Bryan Anderson
January 2, 2026 AT 21:49Thank you for compiling such a comprehensive and well-researched overview. The systemic nature of medication errors is often overlooked in favor of blaming individual providers. The data on IV errors and counterfeit pharmaceuticals is particularly alarming. I would only add that interdisciplinary communication protocols-such as structured handoffs and pharmacist-led med reconciliations-are proven to reduce harm by up to 40% in institutional settings. These are not optional best practices; they are patient safety imperatives.
Liam George
January 4, 2026 AT 19:06Let’s be real-this isn’t about ‘errors.’ It’s about control. The pharmaceutical-industrial complex thrives on confusion. Why do you think they make labels unreadable? Why do they push polypharmacy on seniors? Because dependency is profitable. The FDA? They’re regulated by the same lobbyists who fund their campaigns. Fake fentanyl pills? That’s not a market failure-it’s a feature. They want you scared, dependent, and dosed up. Wake up. The system isn’t broken. It’s working exactly as designed.
And no, your ‘living medication list’ won’t save you. The real solution? Ditch the pills. Go holistic. Or better yet-move to Canada. They’re not lying to their people there.
sharad vyas
January 6, 2026 AT 07:44In India, we don’t have fancy apps or VIPPS seals. We get our medicine from the local shop, and the guy behind the counter knows your family. He remembers if you’re diabetic or have high blood pressure. He tells you not to mix it with tea. No one writes a list. But we survive. Maybe the problem isn’t just the system-it’s how we overcomplicate things. Sometimes, human trust beats digital verification.
Still, fake pills? That’s new. That’s scary.
gerard najera
January 6, 2026 AT 16:181.3 million harmed. 7,000 dead. That’s not a statistic. That’s every hospital wing, every ER bay, every grieving family.
It’s preventable. And we’re not doing enough.
Stephen Gikuma
January 7, 2026 AT 15:41They’re lying about the numbers. You think the government wants you to know how many people they’re killing with bad meds? Nah. They’d rather you blame Big Pharma. But who controls the FDA? Who writes the guidelines? Who gets the contracts? It’s all connected. The fake pills? They’re not coming from some shadowy website-they’re being shipped through customs with paperwork stamped ‘approved.’ You think that’s an accident?
Wake up. This is a war on the middle class. And they’re dosing us into submission.
Bobby Collins
January 8, 2026 AT 03:16okay but like… have you seen the new fentanyl test strips? they’re like $5 on amazon and you just put a tiny bit of the pill in water and it turns blue if it’s laced?? i got mine after my cousin almost died and now i test EVERYTHING. like, even if it’s from my doctor?? yes. even then. i don’t trust anyone anymore 😭
Layla Anna
January 9, 2026 AT 02:41my grandma took her meds wrong for 3 months because the bottle said 'take 1 every 12 hours' but the label said 'take 2x daily' and she thought that meant morning and night... but she took them at 7am and 7pm instead of 8am and 8pm and her kidneys almost gave out
pharmacist didn't catch it because she switched pharmacies last year
we were lucky she didn't die
please use one pharmacy
please
please
please
Heather Josey
January 10, 2026 AT 00:14This is one of the most important public health pieces I’ve read this year. The fact that medication errors surpass car accidents as a leading cause of preventable harm should be front-page news. I’ve trained nurses for over a decade, and I’ve seen the same patterns: fragmented records, rushed consultations, and patients too afraid to ask questions. We need mandatory medication literacy programs in schools, not just for seniors. Empower people early. Knowledge is the only true safety net.
Donna Peplinskie
January 10, 2026 AT 22:52Oh my goodness, thank you for this-seriously, thank you. I’ve been trying to get my sister to keep a meds list for years, and she just rolls her eyes. But now I’m going to print this out and hand it to her with a cup of tea and say, ‘This isn’t nagging. This is love.’
Also, I love that you mentioned Australia’s 5 Moments. I’ve started using that with my dad-he’s 82, on seven meds, and he actually listens to me now because it’s structured, not scary.
You did a beautiful job. 💛
Olukayode Oguntulu
January 12, 2026 AT 14:34Ah, the Western medical-industrial complex-where commodification of health has reached its apotheosis. The pharmacopeia has been reduced to a neoliberal commodity chain, wherein the body becomes a site of algorithmic surveillance and pharmacological governance. The fentanyl-laced counterfeit pills? Merely the symptomatic manifestation of a deeper ontological crisis: the alienation of the patient from the therapeutic process. The solution? Not a list. Not a pharmacy. But a radical re-embodiment of care-decolonizing pharmacology, rejecting the hegemony of the pill, and returning to ancestral modalities of healing. Until then, we are merely patients in a machine designed to consume us.
jaspreet sandhu
January 14, 2026 AT 00:05Everyone is making this too complicated. In my village in Punjab, we never had pills labeled in English. We had our auntie who knew which herb cured what. We didn’t need a list. We didn’t need a pharmacist. We didn’t need a website. We just listened to the elders. Now everyone is scared of their own shadow. You think a test strip will save you? It won’t. You think a VIPPS seal means anything? That’s just another scam to sell you more stuff. The real problem? You stopped trusting people. You stopped asking your neighbor. You started trusting a screen. That’s why you’re getting poisoned. Go back to the old ways. Or at least stop buying pills from people who post on TikTok. That’s just dumb.